Complete Solutions for Snoring Problems: A Comprehensive Guide
Published by Dr. James Wilson | Sleep Medicine Specialist
Key Points:
- 45% of adults snore occasionally, with 25% experiencing chronic snoring
- Snoring can indicate underlying sleep apnea in 30% of cases, requiring medical evaluation
- Snail Sleep APP can help monitor snoring patterns and detect potential sleep apnea
- Lifestyle changes can reduce snoring severity by 40-60% in most cases
- Multiple treatment options available, from simple lifestyle modifications to medical interventions
Summary: Snoring affects nearly half of all adults and can significantly impact both the snorer's and their partner's sleep quality. While often dismissed as a minor annoyance, snoring can indicate serious underlying health conditions. Modern sleep monitoring tools like Snail Sleep APP can help identify patterns, assess severity, and guide appropriate treatment decisions.
 Snoring causes solutions
Snoring causes solutions
Snoring affects millions of people worldwide, disrupting sleep for both the snorer and their bed partner. While often dismissed as a minor annoyance, snoring can be a symptom of underlying health issues and may indicate the presence of sleep apnea, a serious sleep disorder. This comprehensive guide provides a complete roadmap for understanding, diagnosing, and treating snoring problems, offering solutions that range from simple lifestyle changes to advanced medical interventions.
Understanding Snoring: More Than Just Noise
What is Snoring?
Definition:
- Snoring: Sound produced by vibration of soft tissues in the upper airway
- Mechanism: Airway narrowing causes increased airflow velocity and tissue vibration
- Location: Usually occurs in the nose, mouth, or throat
- Timing: Most common during sleep when muscles are relaxed
Physiological Process:
- Airway narrowing: Reduced space for air to pass through
- Increased resistance: Higher pressure needed to move air
- Tissue vibration: Soft tissues vibrate with rapid airflow
- Sound production: Vibration creates characteristic snoring sounds
Types of Snoring:
- Primary snoring: Benign snoring without breathing pauses
- Positional snoring: Only occurs in certain sleep positions
- Snoring with sleep apnea: Associated with breathing pauses
- Complex snoring: Multiple factors contributing to the problem
Health Significance:
- Symptom indicator: Can signal underlying health problems
- Sleep quality: Often indicates poor sleep architecture
- Health risks: May be associated with serious conditions
- Treatment guide: Understanding cause guides treatment approach
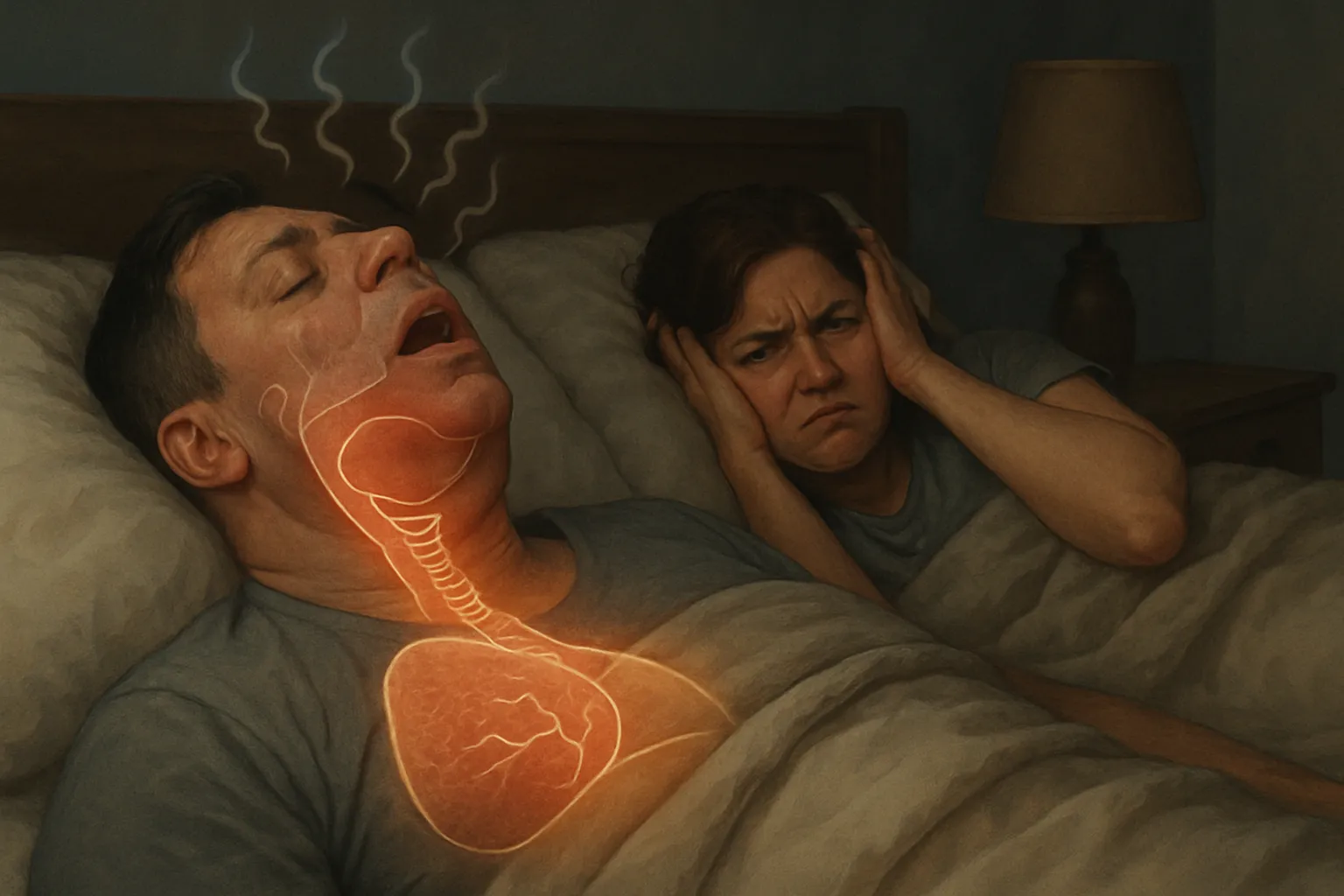 Snoring causes impact
Snoring causes impact
The Impact of Snoring
On the Snorer:
- Sleep disruption: Frequent awakenings during the night
- Sleep quality: Reduced time in restorative sleep stages
- Daytime fatigue: Persistent tiredness and sleepiness
- Health consequences: Increased risk of cardiovascular problems
On the Bed Partner:
- Sleep deprivation: Significant sleep loss due to noise
- Relationship strain: Tension and frustration in relationship
- Health effects: Sleep deprivation affects partner's health
- Quality of life: Reduced enjoyment of shared activities
On Overall Health:
- Cardiovascular risk: Increased blood pressure and heart disease risk
- Metabolic effects: May contribute to weight gain and diabetes
- Immune function: Poor sleep affects immune system
- Mental health: Sleep problems can lead to depression and anxiety
Root Causes of Snoring
Anatomical Factors
Nasal and Sinus Issues:
- Deviated septum: Crooked nasal septum blocking airflow
- Nasal polyps: Soft growths blocking nasal passages
- Chronic sinusitis: Inflammation and mucus blocking nose
- Allergic rhinitis: Swelling and congestion from allergies
Throat and Airway Problems:
- Enlarged tonsils: Large tonsils blocking throat
- Adenoid hypertrophy: Enlarged adenoids behind nose
- Uvula elongation: Long hanging tissue in throat
- Soft palate issues: Thick or long soft palate
Facial Structure:
- Small jaw: Underdeveloped jaw reducing airway space
- Narrow palate: High, narrow roof of mouth
- Large tongue: Tongue too large for mouth
- Retrognathia: Recessed lower jaw
Medical Conditions
Sleep Apnea:
- Obstructive sleep apnea: Complete or partial airway blockage
- Central sleep apnea: Brain not signaling breathing
- Mixed sleep apnea: Combination of both types
- Severity levels: Mild, moderate, or severe
Endocrine Disorders:
- Hypothyroidism: Underactive thyroid causing tissue swelling
- Diabetes: Metabolic changes affecting airway function
- Acromegaly: Excessive growth hormone enlarging tissues
- Obesity: Excess fat around neck and throat
Neurological Conditions:
- Muscular dystrophy: Weak muscles unable to keep airway open
- Multiple sclerosis: Nerve damage affecting muscle control
- Stroke: Brain damage affecting breathing control
- Parkinson's disease: Movement disorder affecting airway muscles
Lifestyle and Environmental Factors
Weight and Body Composition:
- Obesity: Excess weight around neck and throat
- Fat distribution: Fat deposits in airway area
- Muscle tone: Reduced muscle strength with weight gain
- Inflammation: Obesity increases airway inflammation
Sleep Position:
- Supine sleeping: Back sleeping worsens snoring
- Gravity effect: Tissues fall back when on back
- Positional snoring: Only occurs in certain positions
- Treatment response: Often responds to position changes
Alcohol and Medications:
- Alcohol consumption: Relaxes throat muscles
- Sedatives: Medications that relax muscles
- Muscle relaxants: Direct muscle relaxation effects
- Antihistamines: Can cause drowsiness and muscle relaxation
Sleep Environment:
- Room temperature: Too warm or too cold
- Humidity levels: Dry air irritating airways
- Allergens: Dust, pet dander, or mold
- Bed comfort: Uncomfortable mattress or pillows
Comprehensive Diagnostic Approach
Self-Assessment and Monitoring
Sleep Diary:
- Sleep patterns: Record bedtime, wake time, and sleep quality
- Snoring frequency: Note when and how often snoring occurs
- Position correlation: Link snoring to sleep positions
- Symptom tracking: Monitor daytime symptoms and energy levels
Partner Observations:
- Snoring intensity: How loud and frequent the snoring is
- Breathing patterns: Any pauses or gasping sounds
- Sleep quality: Partner's observations of sleep disruption
- Position changes: How position affects snoring
Symptom Checklist:
- Daytime sleepiness: Excessive tiredness during day
- Morning headaches: Frequent morning headaches
- Difficulty concentrating: Problems with focus and attention
- Mood changes: Irritability, depression, or anxiety
Professional Evaluation
Primary Care Assessment:
- Medical history: Complete health evaluation
- Physical examination: Check for anatomical issues
- Risk factor assessment: Identify contributing factors
- Referral coordination: Connect with appropriate specialists
Sleep Medicine Consultation:
- Sleep specialist evaluation: Expert assessment of sleep problems
- Sleep study recommendation: Determine if sleep study needed
- Treatment planning: Develop comprehensive treatment approach
- Follow-up coordination: Plan ongoing care and monitoring
Specialist Consultations:
- Otolaryngologist: Ear, nose, and throat specialist
- Dental sleep medicine: For oral appliance therapy
- Cardiologist: If cardiovascular issues present
- Endocrinologist: For hormone-related problems
Diagnostic Testing
Sleep Study (Polysomnography):
- Comprehensive monitoring: Brain waves, breathing, heart rate, oxygen
- Snoring measurement: Objective measurement of snoring
- Breathing assessment: Check for breathing pauses
- Sleep quality: Detailed analysis of sleep architecture
Home Sleep Apnea Testing:
- Simplified monitoring: Basic breathing and oxygen monitoring
- Convenience: Can be done at home
- Cost-effective: Less expensive than lab studies
- Screening tool: Good for initial assessment
Imaging Studies:
- CT scan: Detailed images of nasal and throat structures
- MRI: Soft tissue imaging for detailed assessment
- X-rays: Basic imaging for structural problems
- Endoscopy: Direct visualization of airway
Laboratory Tests:
- Blood work: Check for underlying medical conditions
- Hormone levels: Assess thyroid and other hormone function
- Inflammatory markers: Check for inflammation
- Metabolic tests: Assess glucose and other metabolic factors
Treatment Solutions: From Simple to Advanced
Lifestyle and Behavioral Modifications
Weight Management:
- Healthy diet: Balanced, calorie-controlled eating plan
- Regular exercise: Physical activity for weight control
- Behavioral support: Professional weight loss guidance
- Long-term maintenance: Sustainable lifestyle changes
Sleep Position Training:
- Side sleeping: Train yourself to sleep on side
- Position awareness: Develop awareness of sleep position
- Habit formation: Build new sleep position habits
- Consistency: Maintain side sleeping throughout night
Sleep Hygiene:
- Consistent schedule: Same sleep-wake times daily
- Bedroom optimization: Cool, dark, quiet environment
- Pre-sleep routine: Relaxing activities before bed
- Technology management: Limit screen time before sleep
Alcohol and Medication Management:
- Alcohol reduction: Limit or avoid alcohol close to bedtime
- Medication review: Check medications that affect sleep
- Timing adjustments: Change timing of medications
- Alternative medications: Switch to medications with fewer side effects
Natural and Home Remedies
Nasal Treatments:
- Saline rinses: Clear nasal passages naturally
- Nasal strips: Open nasal passages externally
- Humidification: Add moisture to dry air
- Allergen control: Reduce exposure to allergens
Throat Exercises:
- Tongue exercises: Strengthen tongue muscles
- Throat muscle training: Improve airway muscle tone
- Singing exercises: Natural way to strengthen throat
- Breathing exercises: Improve breathing control
Herbal Remedies:
- Peppermint: Natural decongestant properties
- Eucalyptus: Helps clear airways
- Ginger: Anti-inflammatory effects
- Honey: Natural throat soother
Essential Oils:
- Eucalyptus oil: Clear breathing and reduce inflammation
- Peppermint oil: Natural decongestant
- Lavender oil: Promote relaxation and better sleep
- Tea tree oil: Antimicrobial properties
Medical Interventions
Oral Appliances:
- Mandibular advancement devices: Reposition jaw to open airway
- Tongue retaining devices: Hold tongue in forward position
- Custom fitting: Made from dental impressions
- Adjustable design: Allow fine-tuning of position
Positional Therapy:
- Positional trainers: Devices that encourage side sleeping
- Backpack devices: Prevent rolling onto back
- Pillow systems: Special pillows that support side sleeping
- Vibrating devices: Alert when rolling onto back
Nasal Interventions:
- Nasal dilators: Open nasal passages internally
- Nasal surgery: Correct structural problems
- Turbinate reduction: Reduce size of nasal structures
- Sinus surgery: Treat chronic sinus problems
Throat Procedures:
- Tonsillectomy: Remove enlarged tonsils
- Adenoidectomy: Remove enlarged adenoids
- Uvulopalatopharyngoplasty: Remove excess throat tissue
- Palate procedures: Various procedures on soft palate
Advanced Treatment Options
CPAP Therapy:
- Continuous positive airway pressure: Gold standard for sleep apnea
- Mask options: Various mask types for comfort
- Pressure titration: Individualized pressure settings
- Compliance monitoring: Track usage and effectiveness
Surgical Interventions:
- Minimally invasive procedures: Radiofrequency ablation, laser procedures
- Traditional surgery: UPPP, tonsillectomy, adenoidectomy
- Implant procedures: Palatal implants, tongue support devices
- Robotic surgery: Advanced surgical techniques
Hypoglossal Nerve Stimulation:
- Implanted device: Small device implanted in chest
- Nerve stimulation: Stimulates tongue muscles during sleep
- Automatic operation: Works automatically during sleep
- Programmable settings: Adjustable for individual needs
Alternative Therapies:
- Acupuncture: Traditional Chinese medicine approach
- Chiropractic care: Address structural issues
- Osteopathic manipulation: Manual therapy techniques
- Biofeedback: Learn to control physiological responses
Treatment Selection and Implementation
Individualized Treatment Planning
Severity Assessment:
- Mild snoring: Simple lifestyle changes may be sufficient
- Moderate snoring: May require medical interventions
- Severe snoring: Often indicates underlying sleep apnea
- Treatment urgency: More severe cases require immediate attention
Cause Identification:
- Anatomical factors: Structural problems requiring medical intervention
- Medical conditions: Underlying health issues needing treatment
- Lifestyle factors: Modifiable behaviors and habits
- Combination causes: Multiple factors requiring comprehensive approach
Personal Factors:
- Lifestyle considerations: Work, travel, and activity requirements
- Comfort preferences: Tolerance for different treatment approaches
- Cost considerations: Insurance coverage and out-of-pocket costs
- Long-term commitment: Willingness to maintain treatment
Treatment Goals:
- Symptom relief: Reduce or eliminate snoring
- Sleep improvement: Better sleep quality and quantity
- Health benefits: Address underlying health issues
- Quality of life: Improve daily functioning and relationships
Combination Approaches
Multiple Treatments:
- Lifestyle + medical: Combine behavioral changes with medical interventions
- Natural + conventional: Integrate natural remedies with medical treatments
- Surgical + behavioral: Surgery followed by lifestyle modifications
- Device + therapy: Medical devices with behavioral therapy
Treatment Sequencing:
- Start with least invasive: Begin with lifestyle changes
- Add treatments gradually: Build comprehensive approach
- Monitor effectiveness: Track improvement and adjust
- Professional guidance: Work with healthcare team
Long-term Management:
- Regular assessment: Monitor treatment effectiveness
- Adjustment needs: Modify approach as needs change
- Prevention focus: Address risk factors proactively
- Ongoing support: Maintain treatment and lifestyle changes
Monitoring and Long-term Success
Effectiveness Assessment
Symptom Monitoring:
- Snoring reduction: Note changes in snoring intensity
- Sleep quality: Track sleep satisfaction and restfulness
- Daytime function: Monitor energy levels and alertness
- Partner observations: Bed partner's observations of improvement
Objective Measures:
- Follow-up sleep study: Repeat study to assess improvement
- Home monitoring: Use home sleep apnea tests
- Health markers: Monitor blood pressure and other health indicators
- Treatment compliance: Track use of treatments
Quality of Life:
- Daily functioning: Assess improvement in daily activities
- Relationship impact: Note changes in relationship quality
- Work performance: Monitor improvement in work function
- Overall satisfaction: Evaluate treatment satisfaction
Maintenance and Prevention
Ongoing Care:
- Regular check-ups: Periodic medical evaluation
- Treatment maintenance: Continue effective treatments
- Lifestyle maintenance: Sustain healthy habits
- Professional support: Ongoing guidance from healthcare team
Prevention Strategies:
- Risk factor management: Address modifiable risk factors
- Healthy habits: Maintain good sleep hygiene
- Weight management: Sustain healthy weight
- Stress management: Ongoing stress reduction
Relapse Prevention:
- Early warning signs: Recognize when problems return
- Immediate intervention: Address problems before they worsen
- Support systems: Use established support networks
- Professional help: Seek help when needed
Special Considerations
Age-Related Factors
Pediatric Snoring:
- Common causes: Enlarged tonsils and adenoids
- Treatment approach: Often surgical intervention
- Monitoring needs: Regular assessment of growth and development
- Family involvement: Parents play crucial role in treatment
Geriatric Snoring:
- Age-related changes: Natural changes in muscle tone and tissue
- Multiple conditions: Often several health problems
- Medication effects: Multiple medications affecting sleep
- Treatment modifications: Adjust for age-related considerations
Comorbid Conditions
Sleep Apnea:
- Diagnosis importance: Rule out sleep apnea in all snorers
- Treatment coordination: Address both conditions simultaneously
- Monitoring needs: Regular assessment of both conditions
- Professional care: Sleep medicine specialist involvement
Cardiovascular Disease:
- Risk assessment: Evaluate cardiovascular risk factors
- Treatment coordination: Address both conditions
- Monitoring needs: Regular cardiovascular assessment
- Lifestyle integration: Heart-healthy lifestyle changes
Mental Health:
- Depression and anxiety: Common in people with sleep problems
- Treatment integration: Address mental health and sleep together
- Professional support: Mental health professional involvement
- Support groups: Connection with others facing similar challenges
Conclusion
Snoring is a complex problem with multiple causes and solutions. While it may seem like a simple annoyance, it can significantly impact your health, relationships, and quality of life. The key to successful treatment is understanding the underlying causes and implementing a comprehensive, individualized approach.
Effective treatment often requires a combination of approaches, from simple lifestyle changes to advanced medical interventions. Working with a comprehensive healthcare team that includes sleep specialists, otolaryngologists, dentists, and other providers can help you develop the most effective treatment plan.
Remember that treatment is not one-size-fits-all, and what works for one person may not work for another. Be patient with the process of finding the right solution, and don't hesitate to try different approaches or combinations of treatments.
With the right approach and support, most people can achieve significant improvement in their snoring and overall sleep quality. Better sleep leads to better health, better relationships, and a better life. Don't let snoring control your life - take control of your sleep and reclaim your health and happiness.
Key Takeaways
- Snoring can be a symptom of underlying health issues requiring medical attention
- Multiple treatment options are available, from lifestyle changes to medical interventions
- Comprehensive evaluation is essential for effective treatment planning
- Combination approaches often provide the best results
- Long-term success requires ongoing monitoring and maintenance
- Professional guidance is crucial for choosing the right treatment approach
- Treatment should be individualized based on cause, severity, and personal factors
- Prevention and early intervention are key to long-term success
🚀 Take Action Now: Your Path to Quieter Nights
Immediate Steps You Can Take
-
Download Snail Sleep APP - Start monitoring your snoring patterns and sleep quality
- Track snoring frequency, intensity, and duration
- Monitor sleep breathing patterns for apnea symptoms
- Get personalized insights based on your sleep data
-
Assess Your Risk Factors - Evaluate the causes mentioned in this guide
- Check for anatomical factors (nasal issues, throat problems)
- Review lifestyle factors (weight, alcohol, sleep position)
- Consider medical conditions that might contribute
-
Consult a Professional - Seek evaluation if snoring is severe or persistent
- Visit a sleep medicine specialist for comprehensive evaluation
- Consider a sleep study to rule out sleep apnea
- Get personalized treatment recommendations
-
Implement Lifestyle Changes - Begin with the most effective modifications
- Maintain a healthy weight through diet and exercise
- Avoid alcohol and sedatives before bedtime
- Establish good sleep hygiene practices
How Snail Sleep APP Can Help
The Snail Sleep APP is specifically designed to address the snoring challenges discussed in this guide:
- Snoring Analysis: Advanced audio analysis detects and measures snoring patterns
- Sleep Apnea Monitoring: Identifies breathing pauses and irregularities
- Sleep Pattern Analysis: Tracks sleep quality and identifies improvement trends
- Smart Alarm: Wakes you at optimal times to reduce sleep disruption
- Sleep Quality Scoring: Provides objective measurements of sleep improvement
- Partner Impact Assessment: Helps evaluate how treatment affects both sleepers
Success Stories
"Snail Sleep APP helped me discover that my snoring was actually a sign of sleep apnea. The app's breathing pattern analysis alerted me to the problem, leading to proper diagnosis and treatment. My sleep quality has improved dramatically, and my partner finally gets a good night's sleep." - David L., Verified User
"After trying various snoring solutions without success, Snail Sleep APP's detailed analysis revealed that my snoring was positional. The app guided me to sleep on my side, and within weeks, my snoring decreased by 80%. My relationship has improved significantly." - Jennifer K., Verified User
References
- American Academy of Sleep Medicine. (2014). International Classification of Sleep Disorders, 3rd Edition.
- American Academy of Otolaryngology. (2021). Snoring and Sleep Apnea: Comprehensive Treatment Guide.
- Sleep Foundation. (2021). Complete Guide to Snoring: Causes, Treatment, and Prevention.
- Mayo Clinic. (2021). Snoring: Diagnosis and Treatment Options.
- Harvard Health Publishing. (2020). Snoring: When It's a Medical Problem.
Related Articles
- Sleep Apnea Treatment Options: From CPAP to Lifestyle Changes
- Sleep Apnea Solutions: Natural Treatment & Lifestyle Changes
- When Snoring Gets Dangerous: Early Warning Signs of Sleep Apnea
