Understanding Restless Leg Syndrome: How It Disrupts Your Sleep
Published by Dr. Emily Parker | Clinical Sleep Psychologist
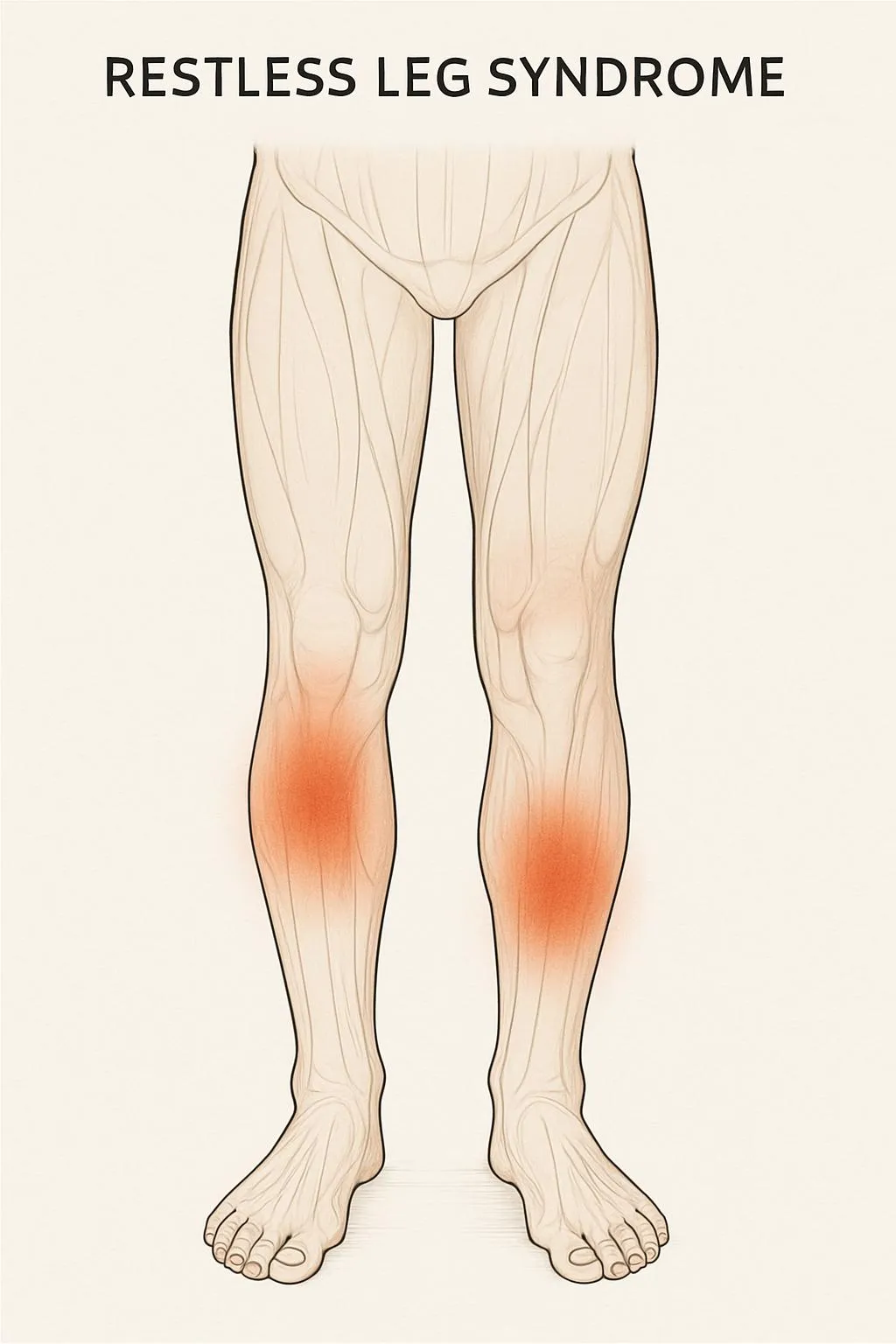 Illustration of legs showing restless leg syndrome symptoms
Illustration of legs showing restless leg syndrome symptoms
Do you experience an irresistible urge to move your legs, especially when trying to fall asleep? You might be suffering from Restless Leg Syndrome (RLS), a neurological condition that affects millions of people worldwide and can significantly impact sleep quality.
Restless Leg Syndrome, also known as Willis-Ekbom Disease, is more than just occasional leg discomfort. It's a legitimate medical condition that can severely disrupt sleep patterns and affect daily functioning. Understanding this condition is the first step toward effective management and better sleep.
What is Restless Leg Syndrome?
Restless Leg Syndrome is a neurological disorder characterized by uncomfortable sensations in the legs and an overwhelming urge to move them. These symptoms typically occur during periods of rest or inactivity, particularly in the evening and nighttime hours.
The International Restless Legs Syndrome Study Group has established four essential criteria for diagnosis:
- Urge to move legs: An uncomfortable urge to move the legs, usually accompanied by unpleasant sensations
- Rest-related symptoms: Symptoms begin or worsen during periods of rest or inactivity
- Movement provides relief: Moving the legs provides temporary relief from discomfort
- Circadian pattern: Symptoms are worse in the evening or night than during the day
Symptoms and Sensations
People with RLS describe their symptoms in various ways, making it sometimes challenging to diagnose. Common descriptions include:
Physical Sensations
- Crawling or creeping feelings inside the legs
- Tingling or pins and needles sensations
- Burning or throbbing pain
- Itching or aching deep within the leg muscles
- Electric shock-like sensations
- Pulling or tugging feelings
Behavioral Symptoms
- Irresistible urge to move legs or feet
- Leg movements during sleep (periodic limb movements)
- Difficulty sitting still for extended periods
- Relief through movement such as walking, stretching, or rubbing legs
- Symptoms worsen in the evening or at bedtime
The Impact on Sleep Quality
RLS significantly affects sleep in multiple ways:
Sleep Onset Difficulties
Most people with RLS experience their worst symptoms when trying to fall asleep. The uncomfortable sensations and urge to move can delay sleep onset by hours, leading to:
- Increased sleep latency (time to fall asleep)
- Frustration and anxiety around bedtime
- Development of anticipatory anxiety about sleep
Sleep Maintenance Problems
RLS often leads to:
- Frequent awakenings during the night
- Difficulty returning to sleep after awakening
- Periodic limb movements during sleep (PLMS), which can occur even when asleep
- Fragmented sleep architecture with reduced deep sleep stages
Daytime Consequences
Poor sleep quality from RLS results in:
- Excessive daytime sleepiness
- Reduced cognitive function and concentration
- Mood changes, including depression and anxiety
- Decreased quality of life and social functioning
Understanding the Causes
RLS can be classified into two main types:
Primary (Idiopathic) RLS
- Genetic component: Up to 90% of people with RLS have a family history
- Brain chemistry: Imbalances in dopamine, a neurotransmitter that controls movement
- Iron deficiency: Low iron levels in specific brain regions
- Age factor: Risk increases with age, though it can affect any age group
Secondary RLS
Secondary RLS is associated with underlying conditions:
Medical Conditions:
- Iron deficiency anemia
- Kidney disease and dialysis
- Diabetes and peripheral neuropathy
- Parkinson's disease
- Rheumatoid arthritis
- Fibromyalgia
Pregnancy: Up to 25% of pregnant women experience RLS, especially in the third trimester
Medications: Certain drugs can trigger or worsen RLS:
- Antihistamines
- Anti-nausea medications
- Antidepressants (particularly SSRIs)
- Antipsychotic medications
- Beta-blockers
Diagnosis Process
Diagnosing RLS primarily relies on clinical evaluation, as there's no specific laboratory test. Healthcare providers use:
Clinical Assessment
- Medical history: Including family history of RLS
- Symptom description: Detailed account of sensations and timing
- Sleep history: Sleep patterns and quality assessment
- Medication review: Current and past medications
Diagnostic Tests
While not specific for RLS, certain tests may be conducted:
- Blood tests: Check iron levels (ferritin, transferrin saturation)
- Kidney function tests: Rule out kidney disease
- Sleep study: May detect periodic limb movements during sleep
Rating Scales
Healthcare providers may use:
- International RLS Rating Scale: Measures symptom severity
- Sleep quality questionnaires: Assess impact on sleep and daily functioning
Treatment Approaches
Treatment for RLS is individualized based on symptom severity, underlying causes, and patient preferences.
Lifestyle Modifications
Sleep Hygiene:
- Maintain regular sleep-wake schedules
- Create a comfortable sleep environment
- Avoid caffeine, especially in the afternoon and evening
- Limit alcohol consumption
Physical Activity:
- Regular moderate exercise can reduce symptoms
- Avoid intense exercise close to bedtime
- Gentle stretching before bed may provide relief
- Yoga and tai chi have shown benefits
Dietary Considerations:
- Ensure adequate iron intake through diet
- Consider iron-rich foods: lean meats, dark leafy greens, legumes
- Avoid large meals close to bedtime
- Some find avoiding certain foods helpful (caffeine, alcohol, artificial sweeteners)
Non-Pharmacological Treatments
Heat and Cold Therapy:
- Warm baths before bedtime
- Heating pads on affected limbs
- Cold compresses for some individuals
- Alternating hot and cold therapy
Massage and Manual Therapy:
- Regular leg massage
- Foam rolling
- Professional massage therapy
- Self-massage techniques before bed
Cognitive Behavioral Therapy:
- Stress reduction techniques
- Relaxation training
- Sleep-focused CBT for associated insomnia
- Mindfulness meditation
Medical Treatments
When lifestyle modifications aren't sufficient, medical treatment may be necessary:
Iron Supplementation:
- Oral iron supplements for deficiency
- Intravenous iron for severe deficiency
- Monitor iron levels to avoid excess
Dopaminergic Medications:
- Pramipexole (Mirapex)
- Ropinirole (Requip)
- Rotigotine patch (Neupro) Note: Long-term use may lead to augmentation (worsening symptoms)
Alpha-2-Delta Calcium Channel Ligands:
- Gabapentin (Neurontin)
- Gabapentin enacarbil (Horizant)
- Pregabalin (Lyrica)
Opioids (for severe, refractory cases):
- Low-dose opioids may be prescribed
- Careful monitoring required due to dependency risk
Sleep Hygiene Specific to RLS
Managing RLS requires specialized sleep strategies:
Evening Routine
- Begin relaxation activities 2-3 hours before bedtime
- Engage in activities that require mental focus (puzzles, reading)
- Practice progressive muscle relaxation
- Use the bathroom before getting into bed to minimize disruptions
Bedroom Environment
- Keep the room cool (around 65-68°F)
- Use comfortable, breathable bedding
- Consider a weighted blanket for some individuals
- Ensure complete darkness with blackout curtains
Managing Nighttime Symptoms
- Keep legs uncovered if this provides relief
- Have a heating pad readily available
- Practice gentle leg exercises if symptoms occur
- Get out of bed if symptoms persist longer than 20 minutes
Technology and Monitoring
Modern sleep tracking technology can help manage RLS:
Sleep Apps like SnailSleep can:
- Track sleep patterns and identify disruptions
- Monitor leg movement patterns during sleep
- Correlate symptoms with environmental factors
- Provide data for healthcare provider discussions
Wearable Devices:
- Track movement during sleep
- Monitor sleep efficiency
- Detect periodic limb movements
When to Seek Professional Help
Consult a healthcare provider if:
- Symptoms occur more than twice per week
- Sleep quality is significantly affected
- Daytime functioning is impaired
- Symptoms worsen or change pattern
- You suspect medication-related RLS
Consider seeing a sleep specialist if:
- Primary care treatment isn't effective
- You need sleep study evaluation
- Complex medication management is required
- You have other sleep disorders
Living with RLS: Long-term Management
Support Networks
- Join RLS support groups (online or in-person)
- Educate family members about the condition
- Connect with others who understand the challenges
Tracking and Documentation
- Keep a symptom diary
- Note triggers and relieving factors
- Track sleep quality and duration
- Document treatment effectiveness
Adaptation Strategies
- Plan activities around symptom patterns
- Choose aisle seats for easier movement during travel
- Inform employers about potential accommodations needed
- Develop coping strategies for symptom flares
The Connection to Other Sleep Disorders
RLS often occurs alongside other sleep conditions:
- Periodic Limb Movement Disorder (PLMD): 80% of RLS patients also have PLMD
- Sleep Apnea: Can coexist with and potentially worsen RLS
- Insomnia: Often develops as a secondary condition
Research and Future Directions
Current research focuses on:
- Better understanding of genetic factors
- Novel dopamine receptor-targeting medications
- Iron metabolism and brain iron regulation
- Non-pharmacological treatment innovations
- Personalized medicine approaches
Conclusion
Restless Leg Syndrome is a real and often debilitating condition that significantly impacts sleep quality and daily functioning. Understanding the symptoms, causes, and available treatments is crucial for effective management.
With proper diagnosis and a comprehensive treatment approach combining lifestyle modifications, non-pharmacological therapies, and when necessary, medical treatment, most people with RLS can achieve significant symptom improvement and better sleep quality.
If you suspect you have RLS, don't hesitate to discuss your symptoms with a healthcare provider. Early intervention and proper management can prevent the condition from significantly impacting your quality of life and sleep health.
Remember, managing RLS is often a journey that requires patience, experimentation with different treatments, and ongoing communication with your healthcare team. With persistence and the right approach, relief is possible.
Keywords: restless leg syndrome, RLS, Willis-Ekbom disease, sleep disruption, leg discomfort, sleep disorders, periodic limb movements
Track your sleep patterns and leg movements with the SnailSleep app to provide valuable data for your healthcare provider.
Related Articles
- Understanding Your Sleep Patterns with Self-Test Questionnaires
- Living with Sleep Apnea: Daily Management and Lifestyle Tips
- Tracking Your Sleep with Technology: A Step-by-Step Guide
