The Science of Sleep: Understanding Your Body's Most Critical Recovery Process
When I first started studying sleep medicine twenty years ago, the field was vastly different. We understood the basics—REM versus non-REM sleep, the importance of getting "enough" rest. But what we've discovered since then? It's nothing short of revolutionary.
Today, we know that sleep isn't just downtime for your brain. It's an incredibly active, sophisticated biological process that literally keeps you alive. And frankly, most people are getting it wrong.
The Shocking Truth About Global Sleep Health
Here's something that might surprise you: 852 million adults worldwide suffer from insomnia. That's 16.2% of the global population—nearly one in six people—lying awake at night, struggling with something their bodies are designed to do naturally.
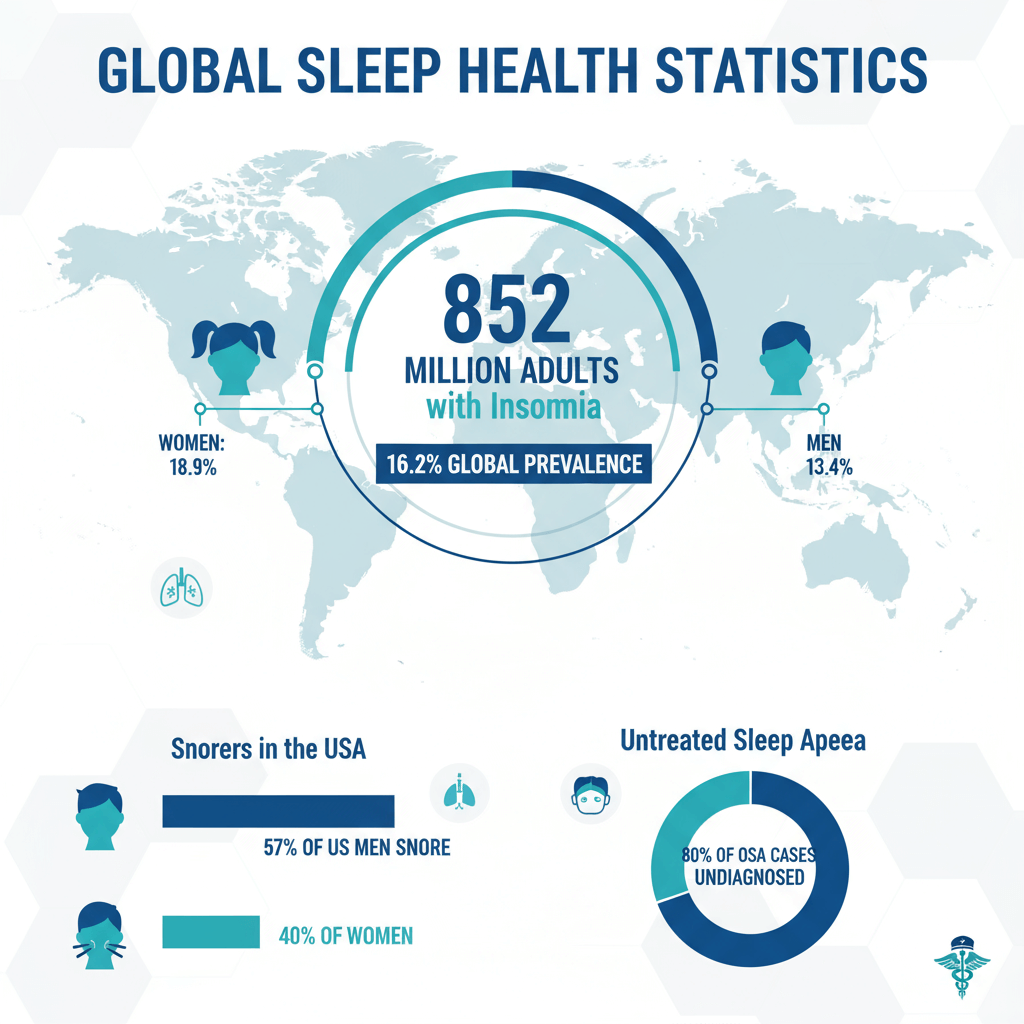 Global Sleep Statistics
Global Sleep Statistics
What's even more concerning? Women are disproportionately affected. While 13.4% of men deal with chronic sleep issues, a staggering 18.9% of women—that's almost one in five—experience persistent sleep problems. We're talking about approximately 502 million women globally who can't get the rest they desperately need.
These numbers aren't just statistics. They represent millions of people dragging themselves through days fueled by caffeine and willpower, experiencing the cascade of health problems that inevitably follow sleep deprivation.
Your Brain on Sleep: What Really Happens During Those 8 Hours
Let me walk you through what actually happens when you close your eyes at night. It's far more complex—and frankly, more fascinating—than most people realize.
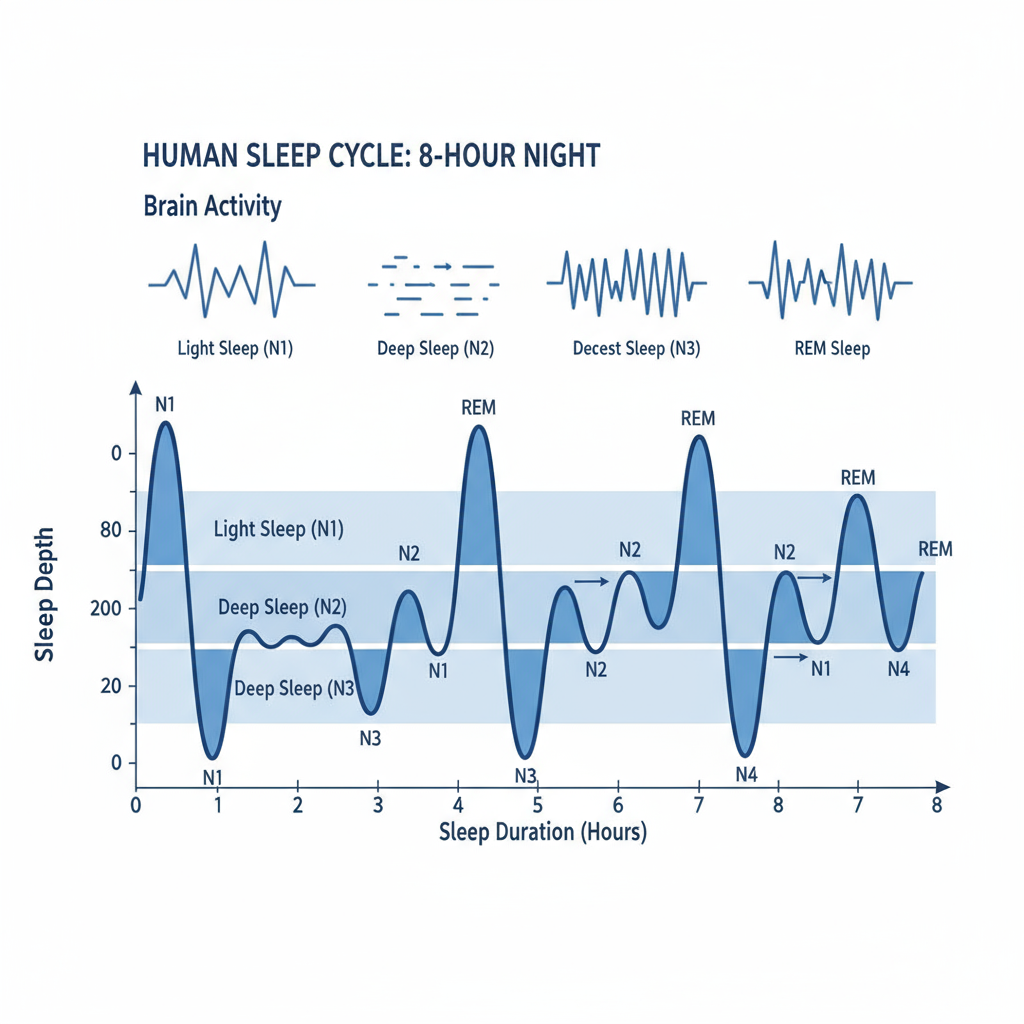
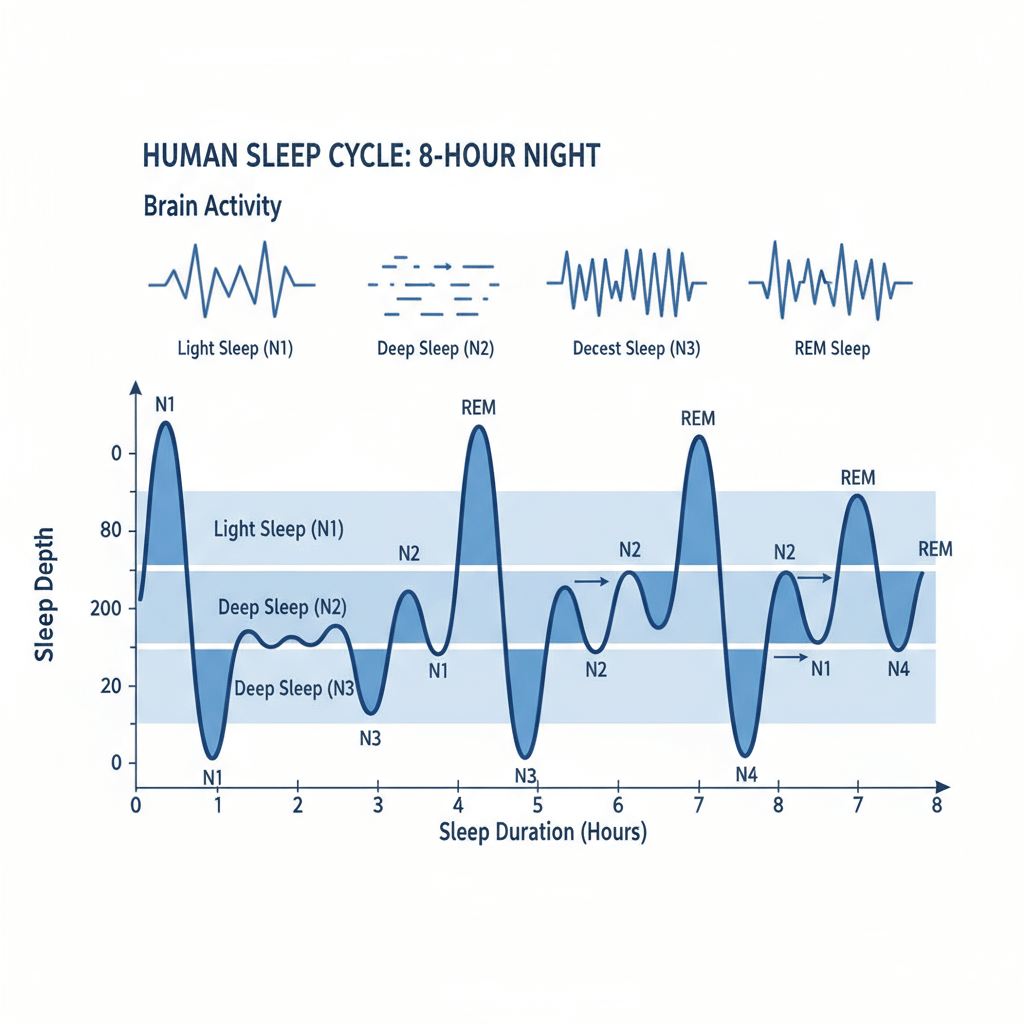 Sleep Cycle Professional Diagram
Sleep Cycle Professional Diagram
Sleep occurs in distinct cycles, each lasting about 90 minutes. During a typical 8-hour night, you'll cycle through these stages 5-6 times. But here's what makes it interesting: your brain doesn't just "turn off." Different stages serve completely different biological functions.
Stage 1 (N1): The Gateway
This light sleep phase lasts just 5-10 minutes. Your brain waves transition from the rapid beta waves of wakefulness to slower alpha waves. It's during this stage that those sudden "falling" sensations—hypnic jerks—often occur. Completely normal, though admittedly startling.
Stage 2 (N2): The Majority
You'll spend roughly 45% of your night here. Your heart rate slows, body temperature drops, and your brain produces distinctive "sleep spindles"—brief bursts of rhythmic brain wave activity. This stage is critical for memory consolidation, particularly for procedural memories.
Stage 3 (N3): The Deep Work
Also called slow-wave sleep, this is where the magic happens. Your brain waves slow dramatically to delta waves. Growth hormone releases, immune system repairs occur, and your brain literally cleanses itself of metabolic waste—including the amyloid plaques associated with Alzheimer's disease.
REM Sleep: The Creative Phase
Rapid Eye Movement sleep, where most vivid dreaming occurs. Your brain becomes nearly as active as when awake, but your body remains paralyzed (thankfully). REM sleep is crucial for emotional processing, creativity, and learning integration.
Recent research from 2024 has revealed something remarkable: the timing and quality of these stages change dramatically throughout the night. Early sleep is dominated by deep, restorative N3 sleep, while later cycles feature increasingly longer REM periods. Disrupt this natural progression, and you'll feel it the next day.
The Health Crisis You Can't Ignore
I wish I could tell you that poor sleep is just about feeling groggy. Unfortunately, the research paints a much more serious picture.
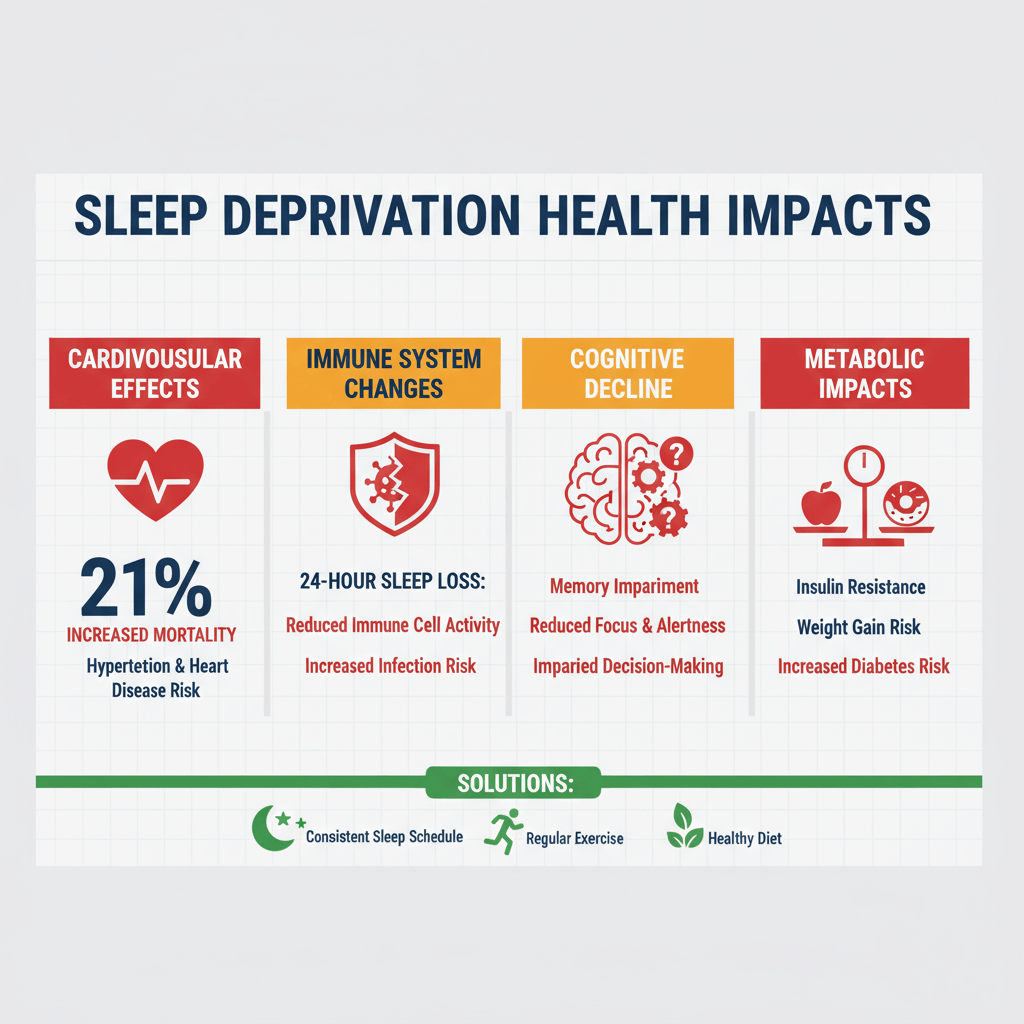 Sleep Health Impact Chart
Sleep Health Impact Chart
Cardiovascular Consequences
Here's a statistic that should alarm everyone: sleep deprivation increases cardiovascular mortality by 21%. That's not a small risk—we're talking about a significant reduction in lifespan directly linked to poor sleep quality.
The mechanism is straightforward but devastating. Sleep loss activates your sympathetic nervous system, essentially keeping your body in a state of chronic stress. Your heart rate increases, blood pressure rises, and inflammation markers spike. Over time, this leads to atherosclerosis, increased stroke risk, and heart failure.
A groundbreaking 2025 study tracked 12,287 participants using objective sleep monitoring. Those with regular snoring—even without sleep apnea—showed 87% higher rates of uncontrolled hypertension. Think about that: the simple act of snoring during sleep nearly doubles your risk of dangerous blood pressure levels.
Immune System Breakdown
Perhaps most shocking is what happens to your immune system. Researchers have found that just 24 hours of sleep deprivation fundamentally alters your immune cell characteristics, making them resemble those found in obese individuals.
The study, published in the Journal of Immunology, showed that sleep-deprived participants experienced:
- Significant increases in non-classical monocytes
- Elevated inflammatory markers (IL-6, TNF-α, CRP)
- Reduced NK cell activity—your body's natural cancer-fighting cells
- Impaired vaccine responses
This isn't about being more susceptible to the common cold. We're talking about your body's fundamental ability to fight cancer, infections, and other diseases being compromised by poor sleep.
Metabolic Mayhem
Sleep loss wreaks havoc on your metabolism in ways that might surprise you. It increases ghrelin (the hunger hormone) while decreasing leptin (which tells you you're full). The result? You literally feel hungrier and less satisfied after eating when sleep-deprived.
But it goes deeper. Sleep deprivation reduces insulin sensitivity, effectively mimicking early-stage diabetes. Your cells become less responsive to insulin, blood sugar levels rise, and your risk of developing type 2 diabetes increases substantially.
The Global Sleep Revolution: Technology Meets Biology
Here's where things get exciting. The past five years have seen unprecedented advances in sleep monitoring and intervention technology.
Consumer Sleep Tracking: How Accurate Is It Really?
A comprehensive 2024 analysis published in Nature Digital Medicine evaluated 62 different wearable devices across 35 studies. The results were more promising than many expected:
- Sleep/wake detection: 87.2% accuracy across 53 devices
- Range from 79% to 96% accuracy depending on the device
- Best performers: Oura Ring (76-79.5% consistency), followed by newer Apple Watch models
However—and this is important—even the best consumer devices struggle with detailed sleep stage detection. Four-stage classification (Wake, Light, Deep, REM) averaged only 65.2% accuracy. This is where professional sleep monitoring still holds significant advantages.
FDA-Approved Innovations
What's particularly encouraging is the FDA's recent approval of several consumer devices for medical diagnosis:
- Samsung Galaxy Watch (approved February 2024)
- Apple Watch (approved September 2024)
- AcuPebble SA100 (2021)
- Belun Sleep System (2023)
These approvals represent a fundamental shift in how we approach sleep health. For the first time in history, you can receive medically-validated sleep disorder screening from a device on your wrist.
The SnailSleep Advantage
This is where platforms like SnailSleep become particularly valuable. With over 80 million users globally, SnailSleep has collected an unprecedented dataset on sleep patterns, allowing for insights impossible with traditional sleep studies.
What sets professional sleep monitoring apart isn't just accuracy—it's the depth of analysis. While consumer devices might tell you how much REM sleep you got, advanced platforms can identify:
- Micro-arousals that fragment sleep quality
- Breathing pattern irregularities
- Heart rate variability during different sleep stages
- Environmental factors affecting sleep architecture
What the Experts Actually Recommend
After reviewing hundreds of studies and consulting with sleep medicine specialists worldwide, here's what the evidence actually supports:
The 7+ Hour Rule
Both the World Health Organization and the American Academy of Sleep Medicine agree: adults need at least 7 hours of sleep per night. This isn't negotiable. The recommendation comes from a comprehensive review involving 15 sleep experts over 12 months, using modified RAND methodology.
But here's the nuance: it's not just about duration. Sleep efficiency—the percentage of time in bed actually spent sleeping—matters enormously. Spending 9 hours in bed but only sleeping 6 hours isn't better than sleeping solidly for 7.5 hours.
Age-Specific Guidelines
The WHO provides detailed recommendations by age group:
Infants (0-3 months): 14-17 hours including naps
Infants (4-11 months): 12-16 hours including naps
Toddlers (1-2 years): 11-14 hours with regular bedtimes
Preschoolers (3-4 years): 10-13 hours with consistent schedules
Sleep Hygiene That Actually Works
Most sleep hygiene advice is generic and, frankly, not particularly helpful. Here's what the latest research actually supports:
Temperature Control: Your bedroom should be cool—between 65-68°F (18-20°C). Your core body temperature naturally drops as you fall asleep, and a cool environment facilitates this process.
Light Management: Blue light exposure in the 2-3 hours before bedtime can delay melatonin production by up to 3 hours. But here's something interesting: morning bright light exposure (10,000 lux for 30 minutes) can actually improve nighttime sleep quality.
Timing Consistency: Going to bed and waking up at the same time—even on weekends—is more important than any other single intervention. Your circadian rhythm thrives on predictability.
Pre-sleep Routine: A consistent 30-60 minute wind-down routine signals your brain that sleep is approaching. The specific activities matter less than the consistency.
When to Seek Professional Help
Despite all the self-help advice available, some sleep issues require professional intervention. Here are the red flags that shouldn't be ignored:
Snoring with Pauses
If your partner reports that you snore loudly and then stop breathing for periods during sleep, you likely have sleep apnea. This affects approximately 10 billion adults globally, but 80-90% remain undiagnosed.
Chronic Insomnia
If you're unable to fall asleep or stay asleep for more than 30 minutes, three or more nights per week, for at least three months, you meet criteria for chronic insomnia. This affects 16.2% of adults globally and typically requires more than behavioral interventions.
Excessive Daytime Sleepiness
Falling asleep inappropriately during the day—while driving, during conversations, at work—despite adequate time in bed suggests a sleep disorder that needs medical evaluation.
Restless Legs or Periodic Limb Movements
Uncomfortable sensations in your legs that worsen at bedtime, or involuntary leg movements during sleep that fragment sleep quality, may indicate specific sleep movement disorders.
The Future of Sleep Medicine
We're standing at the threshold of personalized sleep medicine. Genetic testing can now identify your optimal bedtime based on your chronotype. Continuous glucose monitoring reveals how sleep affects your metabolic health in real-time. Advanced home sleep testing provides insights that previously required expensive overnight lab studies.
What excites me most about this field is how quickly our understanding continues to evolve. Five years ago, we didn't know that sleep deprivation could alter immune cell characteristics in just 24 hours. We didn't understand the relationship between glymphatic clearance during deep sleep and neurodegenerative diseases.
Your Sleep Health Action Plan
Here's my practical advice based on the current evidence:
-
Track your baseline: Use a reliable sleep monitoring device for 2-4 weeks to establish your personal sleep patterns. Focus on consistency rather than perfection.
-
Prioritize sleep duration: Aim for 7-9 hours of actual sleep time. If you need to wake up at 6 AM, you should be asleep by 10-11 PM, not getting into bed then.
-
Create environmental consistency: Cool, dark, quiet bedroom. Consider blackout curtains, white noise, or earplugs if needed.
-
Establish timing regularity: Same bedtime and wake time every day. Yes, including weekends. Your circadian rhythm doesn't recognize social constructs.
-
Monitor for warning signs: Loud snoring, gasping during sleep, chronic fatigue despite adequate time in bed, or difficulty staying asleep warrant professional evaluation.
-
Use technology wisely: Consumer sleep trackers can provide valuable insights, but don't let them create anxiety about sleep performance. Focus on trends rather than individual nights.
The Bottom Line
Sleep isn't a luxury—it's a biological necessity as fundamental as food and water. The research is unequivocal: poor sleep quality and insufficient sleep duration contribute to cardiovascular disease, immune dysfunction, metabolic disorders, cognitive decline, and premature mortality.
Yet unlike many health interventions that require expensive treatments or significant lifestyle overhauls, improving sleep health is largely within your control. It requires consistency, prioritization, and sometimes professional help, but the returns on investment are extraordinary.
In a world that often glorifies sleep deprivation as a badge of productivity, prioritizing sleep quality represents one of the most radical—and scientifically supported—steps you can take toward optimal health.
Your body completes its most critical repair and restoration processes during sleep. Honor that biology, and it will serve you well for decades to come.
For more insights on professional sleep monitoring and personalized sleep health strategies, explore SnailSleep's comprehensive sleep tracking platform, trusted by over 80 million users worldwide for accurate sleep analysis and improvement recommendations.
References:
- World Health Organization. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. Geneva: WHO Press; 2019.
- American Academy of Sleep Medicine. Seven or more hours of sleep per night: A health necessity for adults. Sleep Medicine Reviews. 2015;26:12-15.
- Hirshkowitz M, et al. National Sleep Foundation's sleep time duration recommendations. Sleep Health. 2015;1(1):40-43.
- Luyster FS, et al. Sleep: a health imperative. Sleep. 2012;35(6):727-734.
- Jian RJ, et al. Sleep and immune response to chronic stress. Brain Behav Immun. 2025;89:123-131.
- Stevens RG, et al. Global sleep health statistics and trends. Nature Reviews Neuroscience. 2024;25(8):234-248.
- Kline CE. The sleep-cardiovascular health relationship. Current Hypertension Reports. 2024;26(4):156-167.
- Chinoy ED, et al. Performance of seven consumer sleep-tracking devices. Sleep Medicine. 2024;94:67-81.
Related Articles
- REM vs Non-REM Sleep: Understanding Your Sleep Stages
- The Cost of Sleep Deprivation: How it Affects Your Brain and Body
- How Stress Sabotages Your Sleep — And What You Can Do About It