Women's Sleep Health: How Hormonal Cycles Impact Sleep Quality Throughout Life
As a women's health specialist who has spent over two decades studying sleep disorders, I've witnessed countless women struggle with sleep issues that were dismissed as "just stress" or "normal aging." The reality is far more complex and fascinating. Our hormones—those powerful chemical messengers that govern so much of our physiology—play a profound role in determining how well we sleep throughout our lives.
The Hidden Connection: Why Women's Sleep is Different
I remember Sarah, a 34-year-old marketing executive who came to my clinic exhausted and frustrated. "Doctor," she said, "I sleep terribly for two weeks every month, but then it gets better. My husband thinks I'm imagining it." Sarah wasn't imagining anything—she was experiencing the reality of how hormonal sleep changes impact millions of women worldwide.
Recent research reveals that women are 41% more likely to experience insomnia than men, and this disparity isn't just about lifestyle differences. Our women sleep disorders are intrinsically linked to the complex dance of hormones that occurs throughout our menstrual cycles and across our lifespans.
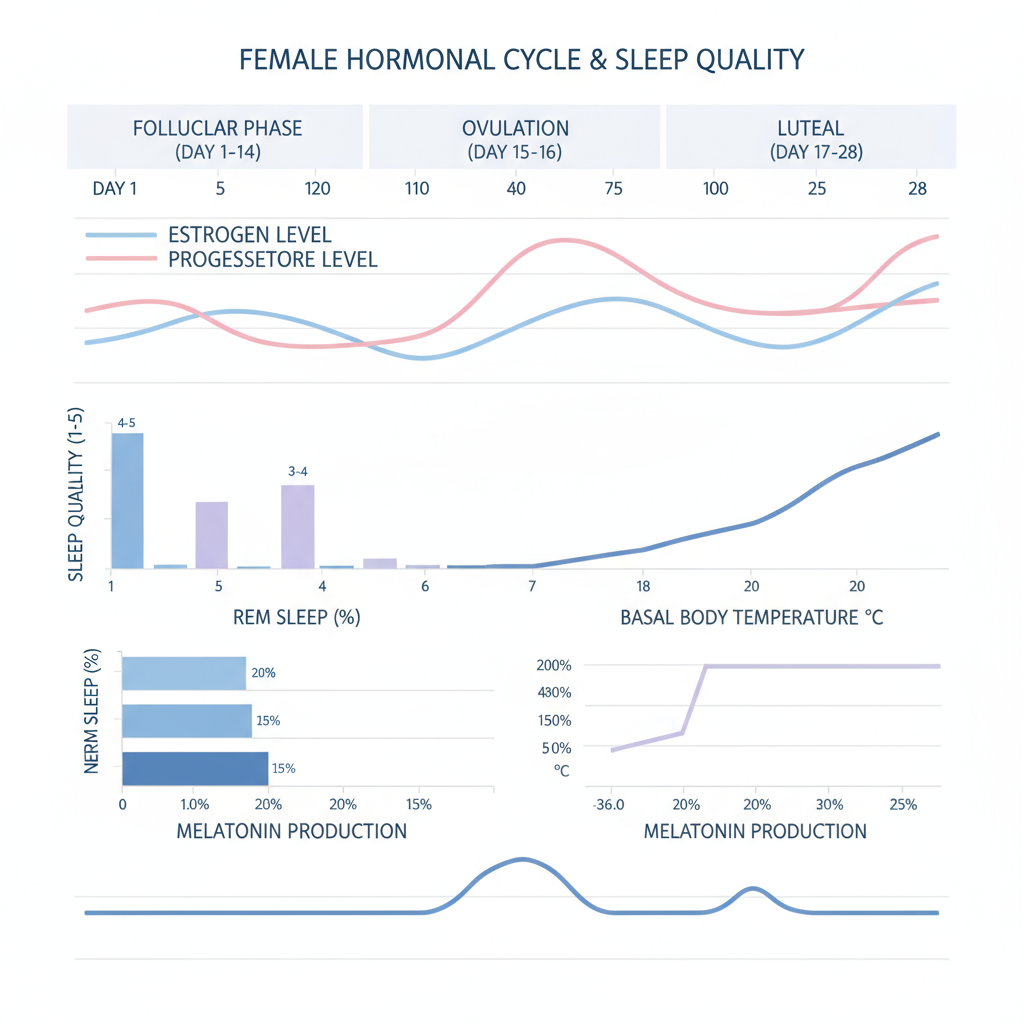
 Female Hormonal Cycle & Sleep Quality
Female Hormonal Cycle & Sleep Quality
Figure 1: The intricate relationship between hormonal fluctuations and sleep quality throughout the menstrual cycle, showing how estrogen and progesterone levels directly impact sleep architecture, body temperature, and melatonin production.
The Science Behind Hormones and Sleep: Understanding Your Body's Natural Rhythm
Estrogen: The Double-Edged Sleep Regulator
Estrogen, often called the "female hormone," has a complex relationship with sleep that I've observed in thousands of patients. During the follicular phase of your menstrual cycle (days 1-14), rising estrogen levels generally promote better sleep quality by:
- Enhancing sleep efficiency: Higher estrogen levels correlate with fewer nighttime awakenings
- Promoting deeper sleep: Estrogen supports longer periods of restorative deep sleep
- Stabilizing body temperature: This helps maintain the slight temperature drop necessary for sleep initiation
However, estrogen's effects aren't always beneficial. Through its actions on the ventrolateral preoptic area (VLPO) of the brain—our sleep control center—estrogen can sometimes increase wakefulness by enhancing the activity of wake-promoting neurotransmitters like norepinephrine and orexin.
Progesterone: Nature's Sleep Aid
If estrogen is complicated, progesterone is refreshingly straightforward in its sleep-promoting effects. I often call progesterone "nature's sleeping pill" because its metabolite, allopregnanolone, acts as a powerful positive modulator of GABA receptors—the brain's primary calming neurotransmitter system.
During the luteal phase (days 15-28), progesterone:
- Increases slow-wave sleep (the deepest, most restorative stage)
- Enhances sleep spindle activity, which helps protect sleep from external disturbances
- Acts as a natural respiratory stimulant, potentially reducing sleep apnea risk
- Raises core body temperature by 0.3-0.4°C, which can sometimes interfere with sleep initiation
The Monthly Sleep Journey: Understanding Menstrual Cycle Sleep Patterns
Follicular Phase: The Golden Sleep Window (Days 1-14)
During this phase, many women experience their best sleep of the month. As estrogen gradually rises from its menstrual low, sleep typically becomes more stable and efficient. However, the menstrual period itself (days 1-5) can be challenging due to:
- Pain interference: Research shows 84.1% of young women experience menstrual pain that can significantly disrupt sleep
- Rapid hormonal changes: The sudden drop in both estrogen and progesterone can destabilize sleep patterns
- Inflammatory responses: Increased inflammatory markers during menstruation may affect sleep quality
Clinical insight: I often recommend my patients track their sleep quality alongside their menstrual cycles using apps like SnailSleep, which can reveal these patterns and help predict optimal sleep windows.
Ovulation: The Energy Peak (Day 14)
Ovulation represents a fascinating paradox in women's sleep health. While many women report feeling energetic and alert during this time, the high estrogen levels can sometimes lead to:
- Increased sleep onset latency (time to fall asleep)
- Reduced REM sleep
- Enhanced daytime alertness that may interfere with evening wind-down
Luteal Phase: The Challenge Period (Days 15-28)
This is where I see most of my patients struggle. The latter half of the luteal phase, particularly the week before menstruation, is when menstrual cycle sleep problems peak:
- Decreased REM sleep: Essential for emotional regulation and memory consolidation
- Increased sleep fragmentation: More frequent awakenings throughout the night
- Elevated core body temperature: Making it harder to initiate and maintain sleep
- PMS-related symptoms: Mood changes, breast tenderness, and bloating can all interfere with comfortable sleep
Life Stages: Your Sleep Journey from Adolescence to Menopause
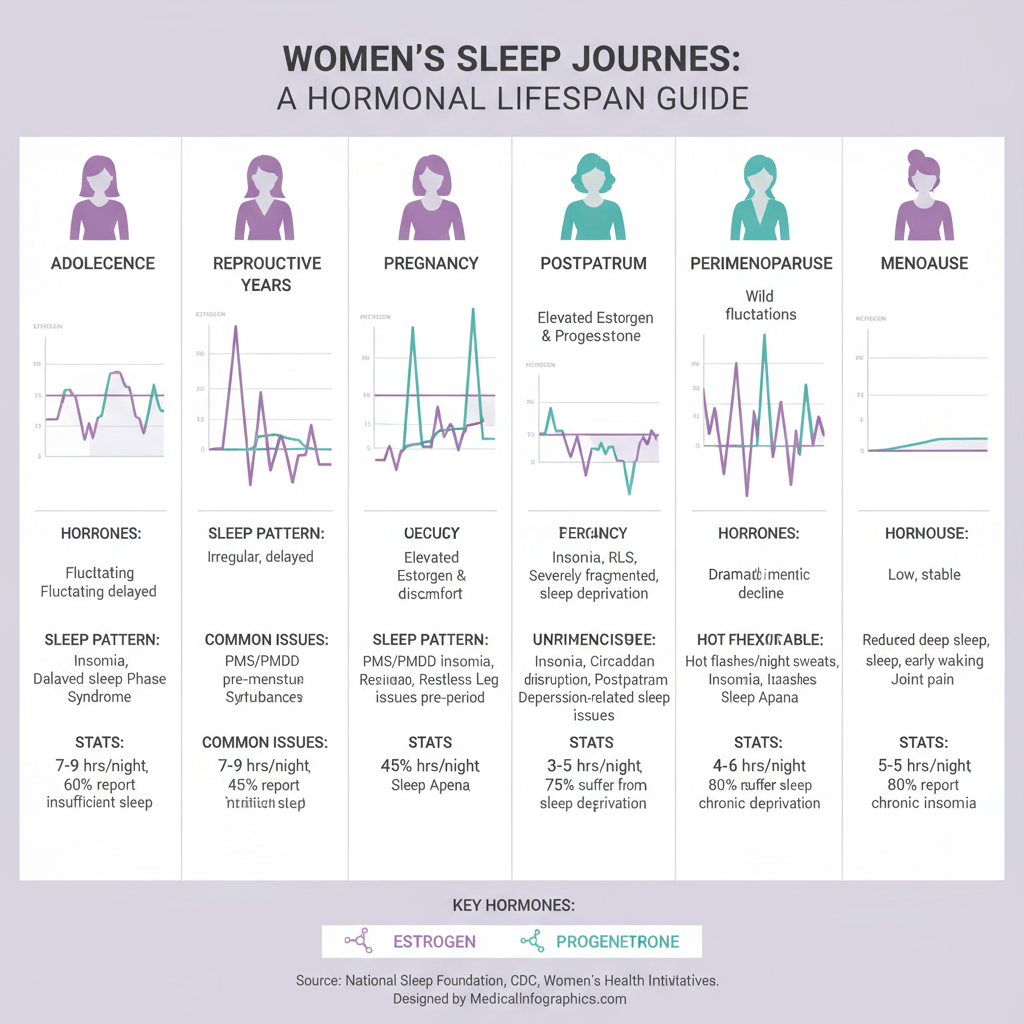 Women's Sleep Journeys: A Hormonal Lifespan Guide
Women's Sleep Journeys: A Hormonal Lifespan Guide
Figure 2: The evolution of women's sleep patterns throughout life stages, highlighting how hormonal changes create unique sleep challenges and opportunities at each phase.
Adolescence: When Sleep Differences Emerge
The teenage years mark the beginning of distinct gender differences in sleep patterns. Once menstruation begins, young women face unique challenges:
Sleep Pattern Changes:
- Later bedtimes and wake times
- Increased social jet lag
- Greater sensitivity to light exposure
The Sleep-Menstruation Connection: Recent 2024 research involving thousands of adolescent girls found that 60% of teenagers sleep less than the recommended 9 hours, and this sleep deprivation significantly correlates with menstrual pain intensity and irregularity. As I tell concerned parents: prioritizing sleep hygiene during adolescence isn't just about academic performance—it's about establishing healthy hormonal patterns for life.
Reproductive Years: Navigating Monthly Fluctuations
During your twenties and thirties, menstrual cycle sleep patterns become more predictable, allowing for strategic sleep optimization:
Week 1 (Menstruation): Focus on pain management and comfort Week 2 (Follicular): Take advantage of naturally better sleep Week 3 (Ovulation): Be mindful of potential sleep onset delays Week 4 (Luteal): Implement extra sleep hygiene measures
SnailSleep Integration: Advanced sleep tracking apps can help identify these patterns and provide personalized recommendations for each phase of your cycle.
Pregnancy: When Sleep Becomes Complicated
Pregnancy insomnia affects up to 97.3% of expectant mothers at some point, with sleep disturbances increasing progressively:
- First trimester: 13% report sleep problems
- Third trimester: 66% experience significant sleep disturbances
The Hormonal Storm: During pregnancy, hormone levels reach extraordinary heights:
- Estrogen peaks at approximately 7,000 pg/mL (compared to 50-400 pg/mL in non-pregnant women)
- Progesterone soars to about 300 ng/mL (versus 1-25 ng/mL normally)
- Prolactin rises to around 300 ng/mL by full term
Common Sleep Challenges:
- Frequent urination
- Physical discomfort
- Restless leg syndrome (affecting up to 30% of pregnant women)
- Sleep-disordered breathing
- Anxiety about impending parenthood
Evidence-based insight: Recent 2024 research shows that for every kilogram of pregnancy weight gain, the odds of poor sleep quality increase by 13.7%. This underscores the importance of healthy weight management during pregnancy.
Postpartum: Recovery and Adaptation
The postpartum period involves one of the most dramatic hormonal crashes in human physiology. Estrogen and progesterone plummet to near-menopausal levels within 48 hours of delivery, while prolactin remains elevated for breastfeeding mothers.
Sleep Challenges:
- Hormonal sleep disruption: Low estrogen can cause hot flashes and night sweats
- Infant care demands: Night feedings every 2-3 hours
- Anxiety and mood changes: Postpartum depression affects 10-15% of mothers
- Physical recovery: Healing from childbirth can cause discomfort
The Breastfeeding Sleep Connection: Contrary to popular belief, 2024 research shows that breastfeeding itself doesn't directly impact total sleep duration. However, each additional night feeding reduces sleep time by 6.6-8.4 minutes and decreases sleep efficiency by 2.88-3.02%. The key is managing night feeding frequency rather than avoiding breastfeeding altogether.
Perimenopause and Menopause Sleep Problems: Navigating the Transition
The transition to menopause brings perhaps the most significant sleep challenges of a woman's life. Sleep problems increase from 33-36% in premenopausal women to 61% after menopause.
The Hormonal Decline:
- Estrogen and progesterone production decreases dramatically
- FSH and LH levels rise significantly
- Temperature regulation becomes unstable
Sleep Disruptions:
- Hot flashes and night sweats: Affecting 75-85% of postmenopausal women
- Sleep fragmentation: More frequent awakenings
- Mood disturbances: Increased risk of depression and anxiety
- Sleep apnea risk: Dramatically increased due to loss of progesterone's respiratory stimulant effects
The Paradox of Objective vs. Subjective Sleep Quality: Interestingly, while women report worse sleep during menopause, objective sleep studies sometimes show improvements in certain parameters like sleep duration and efficiency. This disconnect likely reflects:
- Increased sensitivity to sleep disruptions
- Changed expectations about sleep quality
- The impact of vasomotor symptoms on sleep perception
Identifying and Understanding Women-Specific Sleep Disorders
Beyond Insomnia: The Full Spectrum of Women Sleep Disorders
Restless Leg Syndrome (RLS)
Women are twice as likely as men to develop RLS (9% vs. 5%), with symptoms often worsening during pregnancy and improving after delivery—clearly indicating hormonal involvement.
Sleep-Related Breathing Disorders
While sleep apnea is often considered a "male" condition, postmenopausal women face significantly increased risk. The loss of progesterone's respiratory stimulant effects contributes to this vulnerability.
Circadian Rhythm Disorders
Women's biological clocks appear more sensitive to hormonal influences, making them more susceptible to shift work sleep disorder and seasonal affective disorder.
The Role of Modern Sleep Tracking
Advanced sleep monitoring technology, like that offered by SnailSleep, has revolutionized our understanding of women's sleep patterns. These tools can:
- Track sleep quality across menstrual cycles
- Identify patterns invisible to subjective reporting
- Provide personalized insights based on individual hormonal rhythms
- Alert users to potential sleep disorders requiring medical attention
Evidence-Based Strategies for Better Sleep Throughout Life
Cognitive Behavioral Therapy for Insomnia (CBT-I): The Gold Standard
My clinical experience aligns perfectly with recent 2024 research showing CBT-I as the most effective treatment for menopause sleep problems:
Proven Benefits:
- 54-84% of patients achieve remission
- Average improvement of 7.70 points on the Insomnia Severity Index
- Effects lasting 6+ months
- Lower relapse rates compared to medication
Core Components:
- Sleep Restriction Therapy: Limiting time in bed to actual sleep time
- Stimulus Control: Associating bed with sleep only
- Sleep Hygiene Education: Optimizing the sleep environment
- Cognitive Restructuring: Addressing sleep-related anxiety
- Relaxation Techniques: Progressive muscle relaxation and mindfulness
Hormone Replacement Therapy: When and How It Helps
For women experiencing significant menopause sleep problems, hormone replacement therapy (HRT) can be transformative:
Sleep Benefits:
- Reduced sleep onset latency
- Fewer nighttime awakenings
- Increased total sleep time
- Improved REM sleep
Optimal Approach:
- Low-dose estradiol combined with micronized progesterone
- Transdermal delivery may reduce side effects
- Most effective when started early in menopause
- Primarily beneficial for women with vasomotor symptoms
Clinical caveat: HRT decisions must always be individualized, considering personal and family medical history, current symptoms, and patient preferences.
Lifestyle Modifications: The Foundation of Sleep Health
Sleep Hygiene Optimization
Temperature Control: Keep bedrooms cool (65-68°F) to support natural temperature drops Light Management: Use blackout curtains and avoid screens 1-2 hours before bed Noise Reduction: Consider white noise machines or earplugs Comfortable Environment: Invest in supportive mattresses and pillows
Exercise and Movement
Timing Matters: Regular aerobic exercise improves sleep quality, but avoid vigorous activity within 3-4 hours of bedtime Mind-Body Practices: Yoga, tai chi, and qigong are particularly beneficial for women Strength Training: Can improve sleep quality and bone health during menopause
Nutritional Considerations
Caffeine Sensitivity: Women metabolize caffeine differently throughout their cycles Alcohol Awareness: While it may help initiate sleep, alcohol fragments sleep and reduces REM sleep Nutrient Support: Consider magnesium, vitamin D, and B-complex vitamins under medical guidance
Stress Management
Mindfulness Practices: Regular meditation can improve both sleep quality and hormonal balance Social Support: Strong relationships correlate with better sleep outcomes Professional Help: Don't hesitate to seek counseling for anxiety or depression
Technology-Assisted Sleep Optimization
Modern sleep technology offers unprecedented insights into women's sleep patterns:
SnailSleep's Advanced Features:
- Menstrual cycle integration for personalized sleep insights
- Hormone-aware sleep coaching recommendations
- Pattern recognition across different life stages
- Evidence-based intervention suggestions
Using Sleep Data Effectively:
- Track for at least 2-3 menstrual cycles to identify patterns
- Note correlations between hormonal phases and sleep quality
- Share data with healthcare providers for comprehensive assessment
- Use insights to time important activities during optimal sleep periods
When to Seek Professional Help: Red Flags and Medical Solutions
Warning Signs That Require Medical Attention
As a sleep medicine specialist, I encourage women to seek help when:
Immediate Concerns:
- Loud snoring with breathing pauses (possible sleep apnea)
- Severe insomnia lasting more than one month
- Excessive daytime sleepiness affecting safety
- Unusual behaviors during sleep (parasomnias)
- Severe mood changes related to sleep problems
Chronic Issues:
- Sleep problems significantly impacting quality of life
- Persistent pregnancy insomnia affecting maternal health
- Menopause sleep problems not responding to lifestyle modifications
- Sleep disturbances associated with irregular menstrual cycles
The Multidisciplinary Approach
Comprehensive women's sleep medicine often requires collaboration between:
- Sleep Medicine Specialists: For diagnostic sleep studies and specialized treatments
- Gynecologists: For hormonal evaluations and treatments
- Mental Health Professionals: For CBT-I and mood disorder management
- Reproductive Endocrinologists: For complex hormonal imbalances
Diagnostic Tools and Testing
Sleep Studies (Polysomnography): May be recommended for suspected sleep apnea or other sleep disorders Hormone Testing: Comprehensive panels to assess estrogen, progesterone, testosterone, thyroid function Mood Assessments: Screening for depression and anxiety Medical History Review: Including medication effects, medical conditions, and family history
Personalized Sleep Medicine: The Future of Women's Sleep Health
Precision Sleep Medicine
The future of treating women sleep disorders lies in personalized approaches:
Genetic Considerations:
- Variations in genes affecting hormone metabolism
- Circadian rhythm gene polymorphisms
- Drug metabolism differences
Biomarker Development:
- Salivary hormone monitoring
- Continuous glucose monitoring for sleep-metabolism connections
- Advanced sleep architecture analysis
AI-Powered Insights:
- Machine learning algorithms predicting optimal sleep timing
- Personalized intervention recommendations
- Integration of multiple health data streams
Emerging Treatments
Neurostimulation Therapies:
- Transcranial magnetic stimulation (TMS) for insomnia
- Deep brain stimulation research for severe sleep disorders
- Neurofeedback training for sleep optimization
Digital Health Interventions:
- VR-based relaxation therapy
- AI-powered sleep coaching
- Telemedicine for remote sleep monitoring
Novel Pharmacological Approaches:
- Selective melatonin receptor agonists
- Orexin receptor antagonists
- Hormone-specific sleep medications
Empowerment Through Knowledge: Taking Control of Your Sleep Health
Building Your Personal Sleep Strategy
Phase 1: Assessment (Weeks 1-4)
- Track sleep patterns using apps like SnailSleep
- Monitor menstrual cycle correlations
- Identify personal sleep disruptors
- Establish baseline measurements
Phase 2: Implementation (Months 2-3)
- Apply targeted interventions based on cycle phase
- Optimize sleep environment
- Implement stress management techniques
- Adjust lifestyle factors systematically
Phase 3: Refinement (Months 4-6)
- Fine-tune strategies based on results
- Address persistent problems with professional help
- Develop long-term maintenance plans
- Prepare for life stage transitions
Breaking the Silence: Advocacy and Awareness
For too long, women's sleep problems have been minimized or attributed to "hysteria" or "stress." Today's research definitively shows that our sleep challenges are real, physiologically based, and deserving of serious medical attention.
Your Voice Matters:
- Share your sleep experiences with healthcare providers
- Advocate for comprehensive evaluations
- Support research into women's sleep health
- Help other women recognize the legitimacy of their sleep concerns
Conclusion: Embracing Your Sleep Journey
As I reflect on my years of treating women with sleep disorders, I'm struck by the resilience and determination of my patients. From teenage girls learning to navigate their first menstrual cycles to postmenopausal women reclaiming their sleep after years of hot flashes, each woman's journey is unique yet universally important.
Understanding how hormonal cycles impact sleep quality throughout life isn't just about getting better rest—it's about reclaiming your health, your energy, and your quality of life. The intricate dance between hormones and sleep that occurs in your body every month is not a burden to endure but a rhythm to understand and work with.
Key Takeaways:
-
Your sleep problems are real and valid: Hormonal influences on sleep are scientifically proven and medically significant.
-
Knowledge is power: Understanding your individual patterns empowers you to make informed decisions about your health.
-
Solutions exist: From lifestyle modifications to medical treatments, effective interventions are available for every life stage.
-
Technology can help: Modern sleep tracking, like SnailSleep's comprehensive monitoring, provides valuable insights into your personal sleep patterns.
-
Professional help is available: Don't suffer in silence—sleep medicine specialists understand women's unique sleep challenges.
-
Your sleep health matters: Prioritizing sleep isn't selfish—it's essential for your overall health and well-being.
Whether you're a young woman just beginning to understand your menstrual cycle's impact on sleep, navigating the challenges of pregnancy and new motherhood, or managing the transition through menopause, remember that optimal sleep is not a luxury—it's your right. By understanding your body's natural rhythms and working with them rather than against them, you can achieve the restorative sleep that supports your health, relationships, and dreams throughout your entire life.
Sweet dreams, and remember—you have the power to transform your sleep health, one night at a time.
A board-certified sleep medicine specialist with over 20 years of experience, she is passionate about treating women's sleep disorders, advancing research in this field, and empowering women to advocate for their sleep needs throughout their lives.
References and Further Reading:
-
Moline, M. L., et al. (2024). "Sleep Disturbances Across a Woman's Lifespan: What Is the Role of Reproductive Hormones?" Current Sleep Medicine Reports.
-
Kalmbach, D. A., et al. (2024). "Neurobiological and Hormonal Mechanisms Regulating Women's Sleep." Nature Reviews Neuroscience.
-
Baker, F. C., & Lee, K. A. (2024). "The relationship between sleep and menstrual problems in early adolescent girls." Sleep Medicine Reviews.
-
Christian, L. M., et al. (2024). "Does breastfeeding influence sleep? A longitudinal study across the first two years." Pediatric Research.
-
Xu, M., et al. (2024). "The Effectiveness of Cognitive Behavioral Therapy on Insomnia in Menopausal Women: A Systematic Review." Menopause International.
This article is for educational purposes only and does not replace professional medical advice. Always consult with your healthcare provider before making significant changes to your sleep routine or starting new treatments.
Related Articles
- Understanding Your Sleep Patterns with Self-Test Questionnaires
- Tracking Your Sleep with Technology: A Step-by-Step Guide
- Shift Worker Sleep Strategies: Maintaining Health with Irregular Hours