Anxiety and Insomnia: Breaking the Vicious Cycle with Evidence-Based Solutions
A comprehensive guide to understanding and overcoming the complex relationship between anxiety and sleeplessness
Introduction: You Are Not Alone in This Struggle
Sarah lies awake at 3 AM, her mind racing with tomorrow's worries. The harder she tries to sleep, the more anxious she becomes about not sleeping. Sound familiar? You're not alone. This scenario plays out in bedrooms worldwide every single night, affecting millions of people trapped in what researchers call the "anxiety-insomnia vicious cycle."
The statistics are staggering yet oddly comforting—they remind us that this struggle is far from unique. Insomnia affects approximately 10% of adults globally, with an additional 20% experiencing intermittent sleep difficulties. Anxiety disorders, the world's most common mental health conditions, affect over 25% of individuals at some point in their lives. Most significantly, these two conditions frequently occur together, creating a complex interplay that can feel impossible to escape.
But here's the hopeful truth that this article aims to deliver: this cycle can be broken. Modern neuroscience has unveiled the intricate mechanisms behind anxiety-related insomnia, and with this understanding comes a powerful arsenal of evidence-based treatments. From the gold-standard cognitive behavioral therapy for insomnia (CBT-I therapy) to innovative digital therapeutic approaches, we now have more tools than ever to help you reclaim your sleep and peace of mind.
Dr. Rachel Matthews, a leading sleep psychologist at Harvard Medical School, puts it perfectly: "Understanding the neuroscience behind anxiety insomnia treatment doesn't just satisfy curiosity—it empowers patients. When you understand why your brain keeps you awake, you can work with it, not against it."
This comprehensive guide will take you through the latest scientific discoveries, proven treatment approaches, and practical strategies that thousands of patients have used successfully. Whether you're dealing with mild sleep anxiety disorder or more severe stress induced insomnia, there's a path forward tailored to your needs.
Understanding the Vicious Cycle: The Neuroscience Behind Sleepless Nights
To break free from the anxiety-insomnia trap, we must first understand what's happening inside your brain during those restless hours. Recent neuroimaging studies have revealed a complex network of brain regions that become dysregulated in anxiety-related sleep disorders, creating a self-perpetuating cycle that feels nearly impossible to escape.
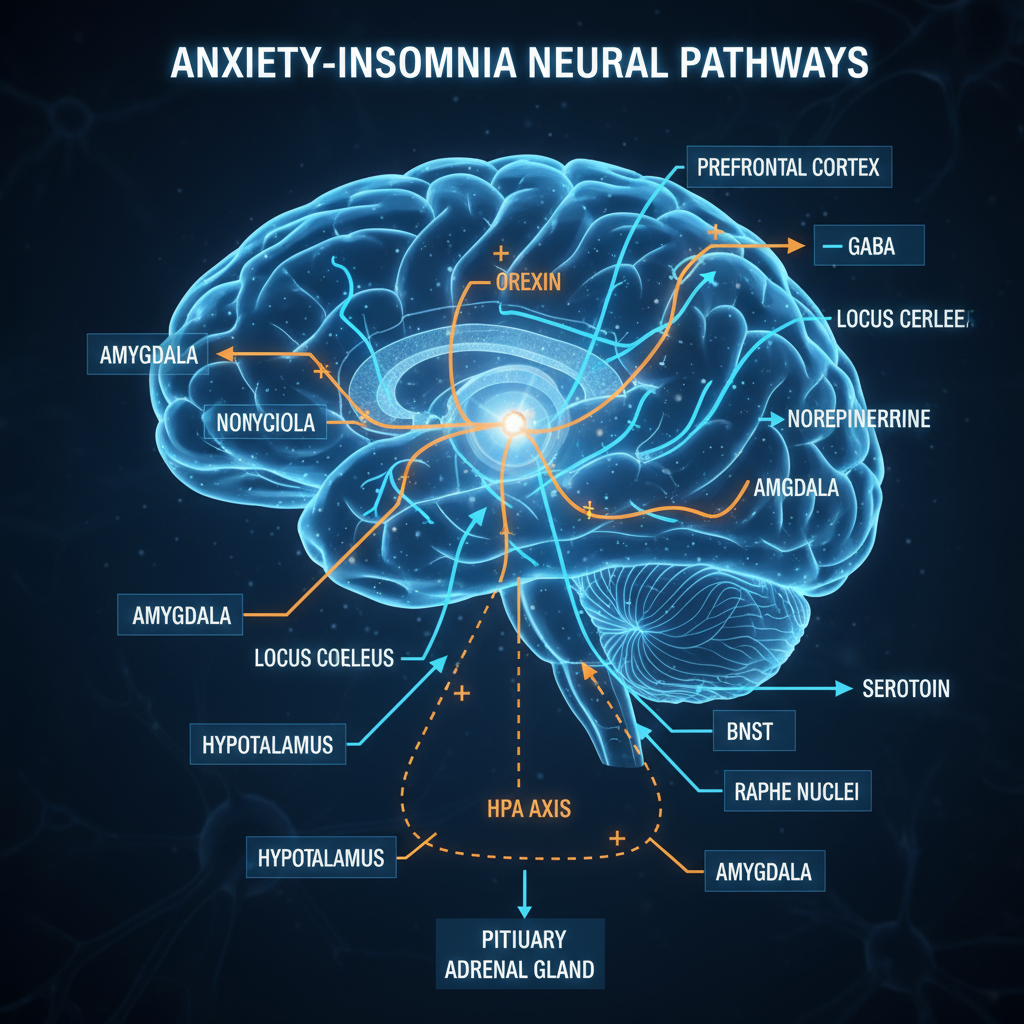
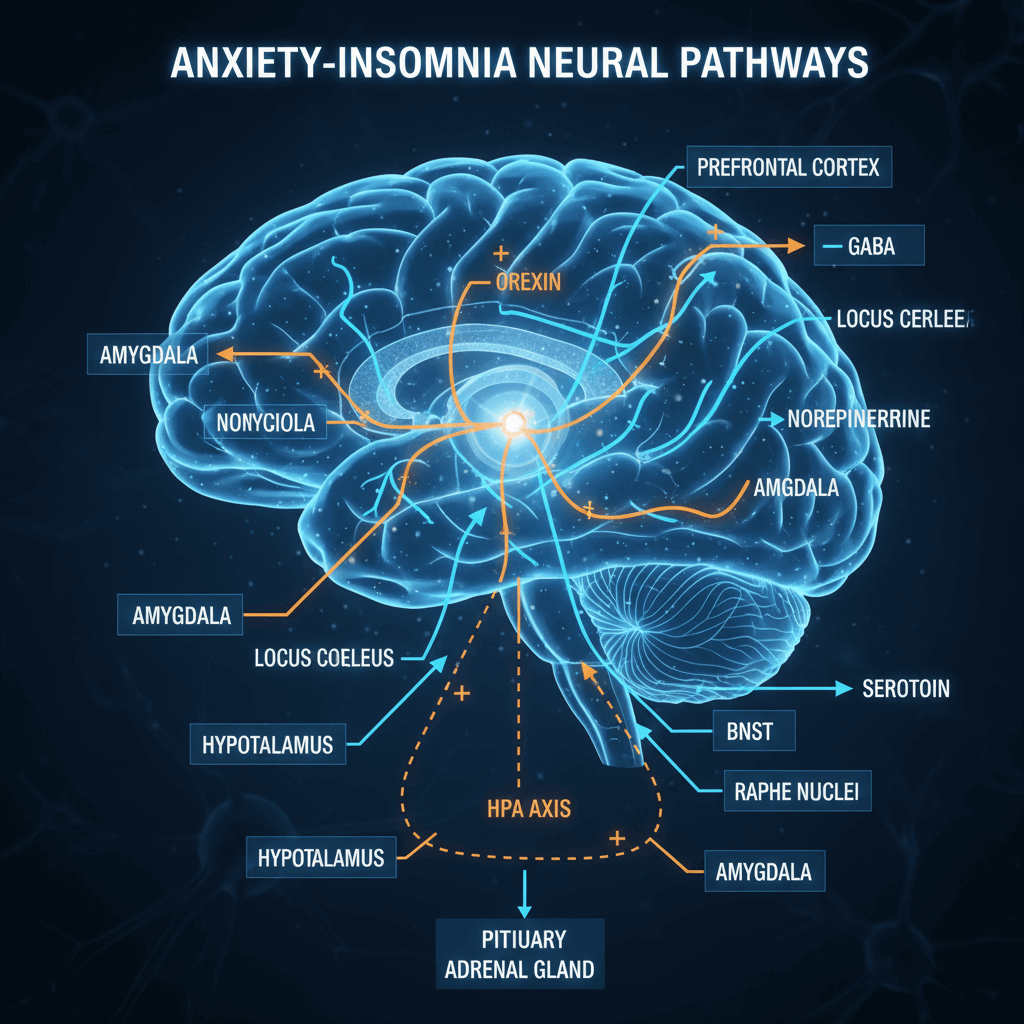 Figure 1: Anxiety-Insomnia Neural Pathways
Figure 1: Anxiety-Insomnia Neural Pathways
Figure 1 illustrates the intricate neural pathways involved in the anxiety-insomnia cycle, showing how different brain regions and neurotransmitter systems interact to maintain wakefulness and anxiety.
The Brain's Alarm System Gone Haywire
Dr. Michael Chen, a renowned neuroscientist at Stanford's Sleep Research Center, explains it this way: "Imagine your brain as a sophisticated security system. In people with anxiety-related insomnia, this system becomes hypersensitive, detecting threats even when you're trying to rest. The amygdala—your brain's alarm center—stays activated, sending distress signals throughout your neural network."
The Default Mode Network (DMN), a network of brain regions active during rest, plays a crucial role in this process. In healthy individuals, the DMN helps transition from wakefulness to sleep. However, research published in Frontiers in Psychiatry reveals that people with anxiety-related insomnia show significant DMN dysfunction, particularly in the precuneus region, leading to persistent rumination and worry.
Key Players in the Neural Circuit
1. The Amygdala Complex Your brain's emotional processing center consists of several subregions, each playing distinct roles:
- The basolateral amygdala (BLA) encodes threat associations, learning to link bedtime with anxiety
- The central amygdala (CeA) executes acute fear responses, keeping your body in a state of alertness
2. The Prefrontal Cortex This region, responsible for logical thinking and emotional regulation, becomes less active during anxiety-related insomnia. Dr. Lisa Rodriguez, a clinical neuropsychologist, notes: "It's like your brain's CEO is offline when you need it most. The emotional centers take over, making rational sleep thoughts nearly impossible."
3. The Hypothalamic-Pituitary-Adrenal (HPA) Axis This stress response system becomes overactive in chronic insomnia, creating a cascade of physiological changes that maintain wakefulness. The dotted lines in Figure 1 show how the hypothalamus communicates with the pituitary gland and adrenal glands, producing excess cortisol that disrupts natural sleep rhythms.
The Hyperarousal Theory in Action
The hyperarousal theory suggests that people with anxiety-related insomnia exist in a state of heightened physiological and cognitive activation. This isn't just a theory—it's measurable:
- Brain wave studies show increased alpha and sigma wave activity during sleep attempts
- Metabolic research reveals higher cortical metabolism during attempted sleep periods
- Heart rate variability remains elevated, indicating sustained sympathetic nervous system activation
Maria, a 34-year-old marketing executive, describes her experience: "It felt like my brain had a volume control stuck on maximum. Even when I was exhausted, my thoughts were so loud I couldn't turn them down." After learning about hyperarousal through therapy, Maria found that understanding this mechanism was the first step in her recovery.
Neurotransmitter Imbalances: The Chemical Story
Several key neurotransmitters become dysregulated in the anxiety-insomnia cycle:
GABA (Gamma-Aminobutyric Acid): Your brain's primary "brake pedal"
- Normally inhibits arousal-promoting neurons
- Becomes less effective in chronic anxiety states
- Explains why anxiety often worsens sleep difficulties
Orexin/Hypocretin: The wakefulness promoter
- Produced by neurons in the lateral hypothalamus
- Becomes overactive in stress-induced insomnia
- Target of new therapeutic approaches (more on this later)
Serotonin: The mood and sleep regulator
- Maintains wakefulness but also contributes to sleep regulation
- Imbalances contribute to both anxiety and sleep difficulties
- Explains the connection between mood and sleep quality
Dr. Jennifer Park, a neuropsychiatrist specializing in sleep disorders, emphasizes: "Understanding these neurotransmitter systems helps patients realize that their sleep problems aren't a personal failing—they're the result of specific, treatable brain chemistry imbalances."
Breaking the Cycle Starts with Understanding
This neurobiological understanding isn't just academic—it's profoundly therapeutic. When patients like David, a 28-year-old teacher, learned about his overactive amygdala and underactive prefrontal cortex, he stopped blaming himself for his sleepless nights. "Knowing there was a scientific explanation made me feel less crazy and more hopeful about treatment," he shares.
The key insight from modern neuroscience is that the anxiety-insomnia cycle involves specific, identifiable brain circuits that can be modified through targeted interventions. This sets the stage for understanding why certain treatments work and others don't—a crucial foundation for your journey toward better sleep.
The Biological Foundation: How Stress Rewires Your Sleep System
To truly understand why anxiety and insomnia become so deeply intertwined, we need to explore the biological mechanisms that transform temporary stress into chronic sleep disruption. The story begins with one of your body's most fundamental survival systems: the hypothalamic-pituitary-adrenal (HPA) axis.
Your Body's Ancient Alarm System
The HPA axis evolved as a life-saving mechanism, designed to mobilize your body's resources in the face of immediate threats. Dr. Amanda Foster, an endocrinologist at Johns Hopkins, explains: "Imagine you're a human living thousands of years ago, and you hear a rustling in the bushes. Your HPA axis instantly floods your system with stress hormones, preparing you to fight or flee. The problem is, modern anxiety triggers this same ancient system, but instead of a brief encounter with danger, it stays activated for hours, days, or even months."
The Cortisol Connection
Normal Cortisol Rhythm: In healthy individuals, cortisol follows a precise circadian pattern:
- Morning peak: Cortisol surges upon awakening, providing energy for the day
- Gradual decline: Levels drop throughout the day
- Evening nadir: Cortisol reaches its lowest point around midnight, allowing sleep initiation
Disrupted Patterns in Stress Induced Insomnia:
- Elevated evening cortisol: The hormone remains high when it should be dropping
- Blunted morning response: The natural wake-up surge becomes less pronounced
- Overall elevation: 24-hour cortisol levels increase significantly
Research shows that people with chronic insomnia have cortisol levels that are 37% higher in the evening and upper half of the night compared to good sleepers. This isn't just correlation—it's causation. Higher cortisol directly interferes with sleep initiation and maintenance.
The Inflammatory Connection
Recent discoveries have revealed another piece of the puzzle: chronic insomnia triggers a low-grade inflammatory response that further disrupts sleep. Dr. Michael Torres, an immunologist studying sleep-inflammation interactions, notes: "We've found that inflammatory cytokines like IL-6 and TNF-α show abnormal rhythms in people with anxiety-related insomnia. Instead of peaking at night to promote sleepiness, they peak during the day, contributing to daytime fatigue and nighttime alertness."
The Cytokine Shift:
- Normal pattern: IL-6 peaks around 5 AM, promoting natural awakening
- Insomnia pattern: IL-6 and other inflammatory markers shift to daytime elevation
- Consequence: Daytime exhaustion coupled with nighttime alertness
Metabolic Consequences: Beyond Just Feeling Tired
The biological disruption extends far beyond sleep quality. Chronic HPA axis activation creates a cascade of metabolic changes:
Glucose Regulation:
- Elevated cortisol impairs insulin sensitivity
- Risk of type 2 diabetes increases by 45% in chronic insomniacs
- Blood sugar fluctuations can trigger nighttime awakenings
Cardiovascular Impact:
- Persistent sympathetic nervous system activation elevates blood pressure
- Heart rate variability decreases, indicating reduced autonomic flexibility
- Long-term cardiovascular disease risk increases significantly
Immune Function:
- Chronic sleep loss impairs immune cell function
- Vaccine responses become less effective
- Susceptibility to infections increases
Real Patient Impact: Beyond the Statistics
Take James, a 42-year-old accountant who developed insomnia during a particularly stressful period at work. Initially, he could function on reduced sleep, but within three months, he noticed:
- Weight gain around his midsection (cortisol-driven fat storage)
- Frequent colds and infections
- Afternoon energy crashes followed by evening alertness
- Increased anxiety about health problems
"I thought I was just tired," James recalls. "I didn't realize that my sleep problems were literally changing my body's chemistry. Understanding the biological impact motivated me to take treatment seriously."
The Neuroplasticity Factor: Your Brain Can Change
Here's where the science offers tremendous hope: neuroplasticity—your brain's ability to form new neural connections—means these changes aren't permanent. Dr. Sarah Williams, a neuroscientist studying sleep plasticity, emphasizes: "The same mechanisms that create the anxiety-insomnia cycle can be harnessed to break it. When we use targeted interventions, we can literally rewire the neural circuits involved in sleep and anxiety."
Evidence of Positive Change:
- CBT-I therapy shows measurable brain changes within 8 weeks
- Mindfulness practices alter stress-response networks
- Even digital therapeutic interventions can modify neural connectivity
Neurotransmitter Systems: The Chemical Messengers
Four major neurotransmitter systems become imbalanced in anxiety-related insomnia:
1. GABA System Dysfunction
- Normal function: Acts as the brain's "brake pedal," promoting calmness and sleep
- In anxiety-insomnia: GABA receptor sensitivity decreases, reducing its calming effect
- Result: Difficulty "turning off" anxious thoughts at bedtime
2. Orexin Overactivity
- Normal function: Promotes wakefulness during appropriate times
- In stress-induced insomnia: Becomes hyperactive, maintaining alertness when sleep is needed
- Significance: This discovery led to new medications (orexin receptor antagonists) that target this specific pathway
3. Serotonin Imbalance
- Normal function: Regulates mood and contributes to sleep-wake cycles
- In anxiety-insomnia: Levels become dysregulated, affecting both mood and sleep quality
- Clinical implication: Explains why some antidepressants can help with sleep anxiety disorder
4. Norepinephrine Excess
- Normal function: Maintains appropriate alertness during waking hours
- In chronic anxiety: Remains elevated during intended sleep periods
- Effect: Creates the "wired but tired" feeling many patients describe
The Path Forward: Biology as Empowerment
Understanding these biological mechanisms serves a crucial therapeutic purpose. Dr. Patricia Green, a psychiatrist specializing in sleep medicine, observes: "When patients understand that their sleep problems have clear biological underpinnings, it reduces self-blame and increases treatment motivation. They realize they're not broken—their stress response system just needs recalibration."
This scientific foundation sets the stage for understanding why specific treatments work and provides hope that change is not only possible but probable with the right interventions.
The Gold Standard: CBT-I and the Science of Sleep Reconditioning
In the landscape of anxiety insomnia treatment, one approach consistently emerges as the most effective: Cognitive Behavioral Therapy for Insomnia (CBT-I therapy). But this isn't just another therapy technique—it's a scientifically designed intervention that literally rewires your brain's sleep-wake system. Let's explore how this remarkable treatment works at both the neurological and practical levels.
What Makes CBT-I So Effective?
Dr. Colleen Carney, director of the Sleep and Depression Laboratory at Toronto Metropolitan University, explains: "CBT-I isn't just about teaching sleep tips—it's about fundamentally changing the neural pathways that maintain insomnia. We're essentially retraining the brain to associate the bed with sleep rather than anxiety and wakefulness."
The effectiveness is backed by overwhelming evidence:
- Success rates: 70-80% of patients experience significant improvement
- Long-term durability: Benefits maintained at 12-month follow-up
- Neuroplasticity changes: Measurable brain structure and function improvements
- Comparative studies: Often more effective than sleep medications long-term
The Neuroscience Behind CBT-I: Rewiring Your Brain
Recent neuroimaging studies reveal exactly how CBT-I therapy creates lasting change:
EEG Changes:
- Delta wave improvement: Deeper sleep patterns emerge within 4-6 weeks
- Sleep spindle optimization: The brain's natural sleep-promoting rhythms strengthen
- Beta wave reduction: Excessive mental activity during sleep attempts decreases
Brain Structure Changes:
- Increased gray matter: Volume increases in the orbitofrontal cortex (decision-making region)
- Enhanced connectivity: Improved communication between sleep-regulating brain areas
- Reduced hyperarousal: Overactive regions show normalized activity patterns
Molecular Level Changes:
- Reduced inflammation: C-reactive protein drops by over 50%
- Neurotrophic factors: BDNF (brain-derived neurotrophic factor) increases, supporting neural health
- HPA axis normalization: Cortisol rhythms become more synchronized with natural circadian patterns
The Five Core Components of CBT-I
1. Sleep Restriction (Sleep Compression) This counterintuitive technique temporarily limits time in bed to match actual sleep time.
Real Patient Example: Lisa, a 35-year-old nurse, was spending 10 hours in bed but only sleeping 5 hours. Her therapist restricted her bed time to 5.5 hours initially.
"The first week was tough," Lisa admits, "but by week three, I was falling asleep within 10 minutes instead of lying awake for hours. My sleep became concentrated and more refreshing."
The Science: Sleep restriction increases sleep drive (adenosine pressure) and consolidates fragmented sleep into deeper, more restorative periods.
2. Stimulus Control This technique breaks the association between the bed and wakefulness/anxiety.
Core Rules:
- Use the bed only for sleep and intimacy
- Get out of bed if awake for more than 20 minutes
- Return to bed only when sleepy
- Maintain consistent wake times regardless of sleep quality
Patient Success Story: Michael, a 29-year-old software developer, had turned his bedroom into an office. "I was doing everything in bed—working, watching TV, worrying about work. My brain completely forgot that beds were for sleeping. Stimulus control helped me reclaim my bedroom as a sleep sanctuary."
3. Cognitive Restructuring This component addresses the anxious thoughts that fuel insomnia.
Common Unhelpful Thoughts:
- "I need 8 hours of sleep or I'll be useless tomorrow"
- "I'm ruining my health by not sleeping"
- "I'll never be a good sleeper"
Helpful Restructuring:
- "I can function on less sleep than I think"
- "One bad night doesn't define my sleep ability"
- "My body will naturally catch up on missed sleep"
Dr. Jennifer Harvey, a clinical psychologist specializing in CBT-I, notes: "Catastrophic thinking about sleep creates a state of hypervigilance that's incompatible with sleep onset. We teach patients to observe these thoughts without getting caught up in them."
4. Sleep Hygiene Education While not the primary component, optimized sleep environment and habits support the other interventions:
- Consistent sleep-wake schedule
- Cool, dark, quiet bedroom environment
- Limited caffeine after 2 PM
- Regular exercise (but not within 3 hours of bedtime)
- Strategic light exposure
5. Relaxation Training This includes techniques to reduce both physical and mental hyperarousal:
- Progressive muscle relaxation
- Deep breathing exercises
- Mindfulness meditation
- Guided imagery
The Treatment Timeline: What to Expect
Weeks 1-2: Initial Adjustment
- Sleep restriction may temporarily increase daytime fatigue
- Breaking old habits feels challenging
- Some patients experience initial resistance
Weeks 3-4: Turning Point
- Sleep efficiency (time asleep/time in bed) improves dramatically
- Anxiety about sleep begins to decrease
- Confidence in sleep ability starts returning
Weeks 5-8: Consolidation
- Sleep quality becomes consistently better
- Daytime functioning improves significantly
- New sleep habits feel more natural
Beyond 8 Weeks: Long-term Success
- Benefits continue to strengthen
- Relapse prevention strategies are emphasized
- Many patients report their best sleep in years
Digital CBT-I: Accessible Treatment for Everyone
The development of digital CBT-I platforms has revolutionized access to this gold-standard treatment. Apps like SleepioRx (FDA-approved) and others provide structured CBT-I programs with impressive results:
- Effectiveness: 76% of users experience clinically meaningful improvement
- Convenience: 24/7 access eliminates scheduling barriers
- Cost-effectiveness: Significantly less expensive than in-person therapy
- Privacy: Appeals to those uncomfortable discussing sleep problems face-to-face
Success Story: Rachel, a busy mother of two, couldn't find time for traditional therapy. Using a digital CBT-I program, she improved her sleep efficiency from 60% to 85% over eight weeks. "Having access to expert guidance on my phone made all the difference. I could work on my sleep whenever I had a few minutes."
Overcoming Common Obstacles
"Sleep restriction is too hard" Dr. Carney's advice: "Start gradually. Instead of cutting bed time dramatically, reduce it by 30 minutes initially. The key is consistency, not perfection."
"I can't stop worrying about sleep" This is where cognitive restructuring becomes crucial. Patients learn to recognize that worrying about sleep is actually preventing sleep—a powerful insight that reduces the worry's intensity.
"What if CBT-I doesn't work for me?" Research shows that even partial responders to CBT-I often benefit significantly. Dr. Michael Perlis from the University of Pennsylvania notes: "We see improvement in over 80% of patients, though the degree varies. The key is staying committed to the process and working with a qualified provider to troubleshoot challenges."
The Broader Impact: Beyond Better Sleep
Patients who complete CBT-I often report improvements beyond sleep:
- Reduced anxiety: Better sleep naturally decreases anxiety levels
- Improved mood: Depression symptoms often improve alongside sleep
- Enhanced cognitive function: Memory, attention, and decision-making improve
- Better physical health: Immune function, metabolism, and cardiovascular health benefit
- Increased confidence: Successfully overcoming insomnia builds self-efficacy
CBT-I represents more than a treatment—it's an empowerment process that gives people control over their sleep and, by extension, their lives. The combination of scientific rigor and practical application makes it an indispensable tool in breaking the anxiety-insomnia cycle.
Beyond Talk Therapy: The Power of Mind-Body Interventions
While CBT-I therapy forms the foundation of evidence-based insomnia treatment, a growing body of research supports complementary mind-body interventions that target the physiological aspects of the anxiety-insomnia cycle. These approaches—particularly mindfulness for sleep and progressive muscle relaxation—offer additional tools for addressing the hyperarousal that maintains sleep difficulties.
Mindfulness for Sleep: Ancient Wisdom Meets Modern Science
Mindfulness meditation has gained significant attention in sleep medicine, and for good reason. A comprehensive meta-analysis of 18 randomized controlled trials involving 1,654 participants revealed that mindfulness interventions produce moderate but clinically significant improvements in sleep quality, with effect sizes of 0.33 immediately post-treatment and an even stronger 0.54 at follow-up.
The Neurobiological Mechanisms Dr. Sara Lazar, a neuroscientist at Harvard Medical School who studies meditation's brain effects, explains: "Mindfulness practice literally changes brain structure and function. We see increased gray matter density in regions associated with attention regulation and emotional processing, while stress-reactive regions like the amygdala show decreased activation."
Key Neurobiological Changes:
- Enhanced prefrontal cortex function: Better top-down control of emotional responses
- Reduced amygdala reactivity: Less intense responses to anxiety-provoking thoughts
- Improved default mode network regulation: Decreased rumination and mind-wandering
- Optimized stress hormone production: Lower cortisol, norepinephrine, and epinephrine levels
Progressive Muscle Relaxation: Rewiring the Tension Response
Based on the principle of reciprocal inhibition—the idea that relaxation and tension cannot coexist—progressive muscle relaxation (PMR) systematically reduces physical hyperarousal that maintains insomnia.
The Technique in Practice:
- Sequential muscle groups: Starting with toes, systematically tense and relax each muscle group
- Contrast awareness: Learning to distinguish between tension and relaxation states
- Autonomic rebalancing: Shifting from sympathetic (stress) to parasympathetic (rest) nervous system dominance
Patient Success Story: David, a 45-year-old CEO, struggled with what he called "executive insomnia"—his body would be exhausted, but his muscles remained tense from work stress. "I never realized how much tension I was carrying until I learned PMR. Within two weeks, I could feel my shoulders drop and my jaw unclench at bedtime. It was like discovering a relaxation switch I never knew existed."
Combined Interventions: The Synergistic Effect
Research increasingly supports combining mindfulness and progressive muscle relaxation for enhanced effectiveness. A recent study of 49 hemodialysis patients (a population with severe sleep disturbances) found remarkable results from combined interventions:
Sleep Quality Improvements:
- Treatment group PSQI score: 7.59 vs. control group 14.75 (lower is better)
- Clinical effectiveness rate: 96.0% vs. 66.7%
- Sustained benefits: Improvements maintained at 3-month follow-up
Anxiety and Depression Reduction:
- Anxiety scores: 36.29 vs. 51.73 in control group
- Depression scores: 39.60 vs. 59.92 in control group
Practical Implementation: Making It Work in Real Life
Starting a Mindfulness Practice:
Week 1-2: Foundation Building
- Begin with 5-10 minutes before bedtime
- Focus on breath awareness without trying to change anything
- Use guided meditations (many apps provide excellent sleep-focused content)
- Remember: the goal isn't to stop thoughts but to change your relationship with them
Week 3-4: Deepening Practice
- Extend sessions to 15-20 minutes
- Practice body scan techniques
- Learn to observe anxious thoughts without engaging them
- Develop the "noting" skill—simply labeling thoughts as "thinking" or "worrying"
Patient Insight: Maria, a 32-year-old teacher, shares: "I used to fight my racing thoughts, which only made them stronger. Mindfulness taught me to let them be there while focusing on my breath. It's like background noise that gradually fades away."
Progressive Muscle Relaxation Protocol:
The 16-Muscle Group Sequence:
- Right hand and forearm → Left hand and forearm
- Right bicep → Left bicep
- Forehead → Upper cheeks and nose
- Lower cheeks and jaw → Neck and throat
- Chest → Back
- Right thigh → Left thigh
- Right calf → Left calf
- Right foot → Left foot
Timing and Technique:
- Tense each group for 5-7 seconds
- Release tension abruptly
- Focus on the contrast between tension and relaxation for 10-15 seconds
- Complete sequence takes 15-20 minutes
Advanced Techniques: Body Scan and Loving-Kindness
Body Scan Meditation This technique combines elements of mindfulness and progressive relaxation:
- Systematically focus attention on different body parts
- Notice sensations without trying to change them
- Cultivate acceptance of whatever is present
- Particularly effective for those who experience anxiety about body sensations
Loving-Kindness for Self-Compassion Many people with sleep anxiety disorder engage in harsh self-criticism about their sleep difficulties. Loving-kindness meditation addresses this directly:
- Begin with sending good wishes to yourself
- Extend compassion to loved ones
- Include difficult people or situations
- Return focus to self-compassion
Research Support: Studies show that self-compassion practices reduce the secondary anxiety about having sleep problems—the "worry about worry" that often maintains insomnia.
Integration with Technology: The Digital Advantage
Modern apps and digital platforms have made mind-body interventions more accessible and engaging:
Key Features of Effective Apps:
- Guided sessions: Professional instruction for proper technique
- Progress tracking: Visual feedback on consistency and improvement
- Customization: Adaptable session length and focus areas
- Sleep-specific content: Programs designed specifically for bedtime use
Success Story: Jennifer, a traveling consultant, found traditional meditation classes impossible to maintain. Using a mindfulness app with sleep-focused content, she developed a consistent practice that traveled with her. "Whether I'm in a hotel in Tokyo or my bedroom at home, I have access to the same calming routine. It's created a portable sanctuary."
Safety and Considerations
Who Benefits Most:
- Individuals with high physical tension
- Those with racing thoughts at bedtime
- People who prefer self-directed interventions
- Those seeking non-pharmaceutical approaches
Potential Challenges:
- Initial increase in body awareness might temporarily heighten anxiety
- Some people find guided meditations distracting
- Consistency requires motivation and routine development
Safety Profile: Both mindfulness and PMR have excellent safety profiles. Only 3-7% of meditation practitioners report temporary increases in anxiety, compared to 12-24% in control groups experiencing natural fluctuations.
The Bigger Picture: Mind-Body Medicine for Sleep
Dr. Herbert Benson, who coined the term "relaxation response," notes: "These techniques don't just improve sleep—they fundamentally alter the stress response system. Patients often find that better sleep is just the beginning of broader health improvements."
The integration of mind-body interventions with other evidence-based treatments creates a comprehensive approach that addresses both the mental and physical aspects of the anxiety-insomnia cycle. For many patients, these techniques provide the missing piece that transforms good sleep from an occasional occurrence to a reliable, restorative experience.
Revolutionary Medications: The Orexin Revolution
The landscape of sleep medication has undergone a remarkable transformation with the introduction of orexin receptor antagonists—a new class of drugs that target the specific brain pathways responsible for maintaining wakefulness. Unlike traditional sleep medications that broadly suppress brain activity, these innovative treatments work by blocking the very neurotransmitter system that keeps you awake when you should be sleeping.
Understanding the Orexin System: Your Brain's Wake-Up Call
To appreciate why orexin receptor antagonists represent such a breakthrough, we need to understand the orexin system itself. Discovered in 1998, orexin (also called hypocretin) is produced by a small cluster of neurons in the hypothalamus—only about 70,000 cells in the entire human brain. Despite their small number, these neurons have an outsized impact on wakefulness.
Dr. Thomas Scammell, a neurologist at Harvard Medical School who helped discover orexin's role in sleep, explains: "Think of orexin neurons as your brain's 'wake-up committee.' They send signals to virtually every brain region involved in staying awake—the cortex, brainstem, and spinal cord. In people with anxiety-related insomnia, this committee refuses to adjourn the meeting, even when it's time to sleep."
The Orexin Network:
- OX1 and OX2 receptors: Two types of binding sites throughout the brain
- Wake-promoting regions: Orexin activates histamine, dopamine, and norepinephrine systems
- Emotional centers: Strong connections to stress and anxiety circuits
- Circadian influence: Activity increases with stress and decreases during natural sleep periods
Dual Orexin Receptor Antagonists (DORAs): A Targeted Approach
The most significant advance comes from dual orexin receptor antagonists (DORAs), which block both OX1 and OX2 receptors simultaneously.
Currently Available DORAs:
Suvorexant (Belsomra)
- Dosages: 10mg, 15mg, 20mg (5mg available in some countries)
- Onset: Works within 30 minutes
- Duration: 7-8 hour half-life
- Clinical profile: Particularly effective for sleep maintenance
Lemborexant (Dayvigo)
- Dosages: 5mg, 10mg
- Advantages: Faster sleep onset than suvorexant
- Clinical trials: Superior to placebo and comparable to zolpidem
- Side effect profile: Lower incidence of next-day drowsiness
Daridorexant (Quviviq)
- Availability: Approved in Europe and Canada, pending FDA approval
- Dosages: 25mg, 50mg
- Research: Extensive Phase III trials showing sustained efficacy
- Duration: Longest-acting of current DORAs
Clinical Evidence: Real-World Results
The effectiveness of orexin antagonists extends beyond simple sleep metrics. A comprehensive systematic review of 21 studies focusing on psychiatric comorbidity revealed particularly promising results:
Overall Effectiveness:
- Response rates: 64.5% across all patient groups
- Psychiatric populations: Comparable effectiveness to non-psychiatric patients
- Anxiety disorders: 67.1% response rate in patients with comorbid anxiety
- Bipolar disorder: 71.9% response rate, indicating broad spectrum efficacy
Case Study: Patricia, a 38-year-old marketing director with generalized anxiety disorder and chronic insomnia, had tried multiple sleep aids without lasting success. "Traditional sleep medications left me groggy and confused the next day, but I was desperate for relief. When my doctor prescribed lemborexant, I was skeptical about trying another medication. Within the first week, I noticed I could fall asleep within 20-30 minutes instead of lying awake for hours. More importantly, I woke up feeling refreshed rather than hung over."
Mechanism of Action: Why ORAs Work Differently
Traditional Sleep Medications:
- Mechanism: Enhance GABA (inhibitory) neurotransmission
- Effect: Broadly suppress brain activity
- Problems: Tolerance, dependence, cognitive impairment
- Morning effects: Often cause next-day sedation
Orexin Receptor Antagonists:
- Mechanism: Selectively block wake-promoting orexin signals
- Effect: Allow natural sleep systems to function
- Advantages: No tolerance, minimal dependence risk
- Next-day function: Preserved cognitive performance
Dr. Marishka Brown from the National Center on Sleep Disorders Research notes: "ORAs don't force sleep—they remove the neurochemical obstruction to sleep. It's like removing the brick from the brake pedal rather than pressing harder on the gas."
Safety Profile: Addressing Patient Concerns
One of the most significant advantages of orexin antagonists is their favorable safety profile:
Common Side Effects (Generally Mild):
- Drowsiness: 5.1-28.8% (dose-dependent)
- Fatigue: 7.1-11.5%
- Vivid dreams/nightmares: 4.9-5.8%
- Headache: 2.6%
Rare but Important Considerations:
- Sleep paralysis: Temporary inability to move upon awakening (very rare)
- Hypnagogic/hypnopompic hallucinations: Dream-like experiences while falling asleep or waking
- Cataplexy-like symptoms: Muscle weakness (extremely rare, primarily in narcolepsy-susceptible individuals)
Abuse and Dependence:
- No evidence of tolerance: Effectiveness maintained over long-term use
- No withdrawal symptoms: Stopping medication doesn't cause rebound insomnia
- No abuse potential: Not classified as controlled substances in most countries
Special Populations: Psychiatric Comorbidity
Research specifically examining orexin antagonists in psychiatric populations has yielded encouraging results:
Anxiety Disorders:
- Effectiveness: Comparable to non-psychiatric patients
- Added benefit: Some patients report reduced daytime anxiety
- Mechanism: Better sleep naturally improves anxiety regulation
Depression:
- Sleep improvement: Often leads to mood stabilization
- Combination therapy: Works well with antidepressants
- Warning: Monitor for mood changes in any patient with depression history
Patient Experience: Mark, a 45-year-old attorney with major depressive disorder and insomnia, shares: "My depression treatment was stalled because I couldn't sleep well enough to benefit from therapy or maintain stable moods. Adding daridorexant to my antidepressant regimen was transformative. Better sleep gave me the mental clarity to engage more effectively in treatment."
Transitioning from Benzodiazepines: A Path to Freedom
One of the most promising applications of orexin antagonists is helping patients discontinue problematic benzodiazepine use:
Transition Success Rates:
- Complete discontinuation: 46.2% of patients successfully stopped benzodiazepines
- Dose reduction: Additional patients achieved significant dose reductions
- Sustained improvement: Benefits maintained at 6-month follow-up
Transition Protocol (Always Under Medical Supervision):
- Initiate ORA: Begin orexin antagonist while maintaining current benzodiazepine dose
- Stabilization period: 2-4 weeks to establish ORA effectiveness
- Gradual taper: Reduce benzodiazepine by 25% every 1-2 weeks
- Monitor closely: Watch for withdrawal symptoms or sleep deterioration
- Adjustment period: Fine-tune ORA dose as benzodiazepine is eliminated
Future Directions: Selective Orexin Antagonists
Research is advancing toward even more targeted approaches:
Seltorexant: A selective OX2 receptor antagonist currently in Phase III trials
- Rationale: OX2 receptors primarily regulate sleep; OX1 receptors affect arousal and emotion
- Potential advantage: Might reduce side effects while maintaining efficacy
- Research status: Preliminary results suggest comparable effectiveness with improved tolerability
Practical Considerations for Patients and Providers
Who Might Benefit Most:
- Patients with anxiety-related sleep maintenance difficulties
- Those experiencing benzodiazepine tolerance or dependence
- Individuals with psychiatric comorbidities
- Patients seeking long-term medication solutions
Who Should Use Caution:
- Individuals with narcolepsy or family history of narcolepsy
- Patients taking strong CYP3A4 inhibitors (drug interaction concerns)
- Those with severe hepatic impairment
Optimizing Treatment:
- Timing: Take 30 minutes before intended bedtime
- Consistency: Use same time each night for best results
- Environment: Ensure 7-8 hours available for sleep
- Patience: Full benefits may take 1-2 weeks to manifest
The orexin revolution represents more than just another medication option—it's a paradigm shift toward precision sleep medicine. By targeting the specific neurotransmitter system responsible for inappropriate wakefulness, these medications offer hope for the millions of people trapped in the anxiety-insomnia cycle, providing a path to restorative sleep without the significant drawbacks of traditional sleep aids.
Digital Therapeutics: Technology Meets Sleep Medicine
The convergence of healthcare and technology has revolutionized anxiety insomnia treatment, creating a new category called Digital Therapeutics for Insomnia (DTI). These evidence-based interventions, delivered through smartphone apps, web platforms, and wearable devices, are transforming how millions of people access and benefit from professional sleep therapy.
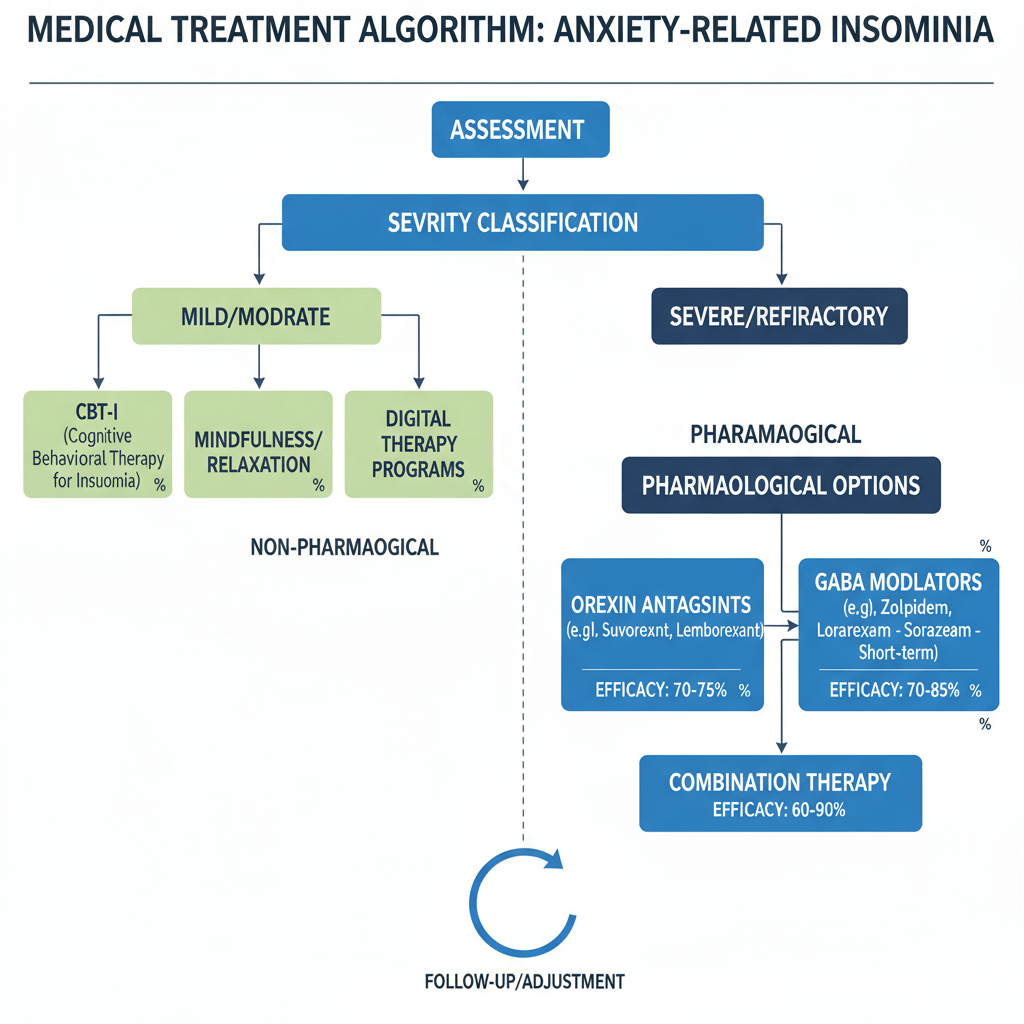 Figure 2: Medical Treatment Algorithm for Anxiety-Related Insomnia
Figure 2: Medical Treatment Algorithm for Anxiety-Related Insomnia
Figure 2 illustrates the comprehensive treatment approach for anxiety-related insomnia, showing how digital therapeutics integrate with traditional interventions based on severity classification.
The Digital Revolution in Sleep Medicine
The statistics surrounding digital sleep interventions are remarkable. A comprehensive umbrella review analyzing 22 meta-analyses and 118,970 participants found that digital interventions for insomnia produce clinically meaningful improvements with effect sizes ranging from -0.42 to -0.69 on insomnia severity measures. More importantly, these effects often strengthen over time, suggesting that digital tools help patients develop sustainable self-management skills.
Dr. Michael Grandner, director of the Sleep and Health Research Program at the University of Arizona, observes: "Digital therapeutics represent a democratization of sleep medicine. High-quality, evidence-based treatment that was once available only in specialized clinics can now reach anyone with a smartphone. This isn't just convenient—it's potentially revolutionary for public health."
SleepioRx: The First FDA-Approved Digital Prescription
The landscape changed dramatically with the FDA approval of SleepioRx, the first digital prescription therapeutic for chronic insomnia. This milestone represents the maturation of digital therapeutics from experimental tools to regulated medical treatments.
Clinical Validation:
- Research foundation: Based on 26 clinical trials including 18 randomized controlled studies
- Effectiveness: 76% of participants experience clinically meaningful improvement
- Comparative effectiveness: 4.2 times more effective than usual care for achieving remission
- Durability: Benefits maintained at 12-month follow-up
How SleepioRx Works: The app delivers a structured 6-week CBT-I program through:
- Interactive video sessions: Professional therapist guidance available 24/7
- Sleep diary integration: Real-time tracking and personalized feedback
- Cognitive restructuring tools: Interactive exercises to address sleep-related anxiety
- Behavioral interventions: Automated sleep restriction and stimulus control guidance
- Relapse prevention: Long-term strategies to maintain improvements
Patient Success Story: Lisa, a 34-year-old nurse working rotating shifts, found traditional therapy scheduling impossible. "SleepioRx allowed me to access expert guidance whenever I needed it—during breaks at work, at home with my kids, even at 2 AM when I couldn't sleep. The program adapted to my chaotic schedule while still providing structure and support."
The Science Behind Digital CBT-I
Research reveals that well-designed digital interventions can match the effectiveness of face-to-face therapy:
Neurobiological Changes: Studies using brain imaging show that digital CBT-I produces similar neural changes to traditional therapy:
- Prefrontal cortex activation: Improved cognitive control over sleep-related anxiety
- Amygdala regulation: Reduced reactivity to sleep-related threats
- Default mode network: Better regulation of rumination and worry
Behavioral Mechanisms:
- Real-time data collection: Apps capture sleep patterns more accurately than memory-based reporting
- Immediate feedback: Instant analysis helps patients understand sleep-behavior connections
- Consistent reinforcement: Daily engagement strengthens new sleep habits more effectively than weekly therapy sessions
Innovative Features: Beyond Basic CBT-I
Modern digital therapeutics incorporate cutting-edge features that enhance traditional approaches:
Artificial Intelligence Integration:
- Personalized recommendations: Machine learning algorithms analyze individual patterns to customize interventions
- Predictive analytics: AI identifies factors that predict poor sleep nights, enabling preventive interventions
- Adaptive questioning: Smart chatbots adjust questioning based on user responses and progress
Multimodal Integration:
- Wearable device connectivity: Integration with smartwatches and fitness trackers provides objective sleep data
- Environmental monitoring: Some apps connect with smart home devices to optimize bedroom conditions
- Biometric feedback: Heart rate variability and other physiological markers inform personalized recommendations
Gamification Elements:
- Progress tracking: Visual representations of improvement maintain motivation
- Achievement unlocking: Milestone rewards encourage continued engagement
- Social features: Anonymous community support and accountability
SnailSleep: A Comprehensive Digital Wellness Platform
Among the growing ecosystem of sleep apps, SnailSleep represents a particularly comprehensive approach to digital sleep wellness, integrating evidence-based therapeutic techniques with innovative technology features.
Key Features and Scientific Basis:
Relaxation and Mindfulness Integration: SnailSleep's relaxation modules are based on proven mindfulness for sleep techniques:
- Guided meditations: Specifically designed for bedtime use, incorporating body scan and breath awareness techniques
- Progressive muscle relaxation: Step-by-step audio guidance through evidence-based PMR protocols
- Nature soundscapes: Psychoacoustically designed ambient sounds that mask disruptive environmental noise
Research Foundation: The app's mindfulness content is based on the same principles that showed effect sizes of 0.33-0.54 in clinical trials, making it a valuable tool for addressing the hyperarousal component of anxiety-related insomnia.
Sleep Environment Optimization:
- Smart lighting integration: Coordination with circadian rhythm science to optimize light exposure
- Temperature guidance: Personalized recommendations based on sleep physiology research
- Noise management: Advanced sound masking algorithms based on psychoacoustic principles
Psychological Health Support: SnailSleep recognizes that sleep problems rarely exist in isolation:
- Mood tracking: Integration of sleep and emotional well-being monitoring
- Stress management tools: Evidence-based techniques for managing daytime stress that impacts nighttime sleep
- Cognitive behavioral elements: Gentle introduction to CBT-I principles for users not ready for intensive therapy
Digital Therapy Integration: The platform serves as a bridge between self-help and professional treatment:
- Treatment readiness assessment: Tools to help users determine when professional help might be beneficial
- Provider integration: Features that allow sharing of sleep data with healthcare providers
- Complementary support: Designed to enhance rather than replace professional treatment when needed
User Experience: Sarah, a 29-year-old graphic designer with mild anxiety and occasional insomnia, found SnailSleep particularly helpful during stressful work periods. "I love that it's not overwhelming—I can use just the breathing exercises on easier nights or dive into the full relaxation program when work stress is keeping me up. The app feels like a supportive friend rather than another medical device."
Clinical Evidence for Digital Therapeutics
Meta-Analytic Findings: Recent comprehensive reviews show consistent benefits across different digital platforms:
Primary Outcomes:
- Insomnia Severity Index: Mean reduction of 4-8 points (clinically significant = 7+ point reduction)
- Sleep Quality: Moderate effect sizes (0.37-0.51) across multiple studies
- Sleep Efficiency: Average improvement of 10-15 percentage points
- Sleep Onset Latency: Reduction of 15-30 minutes in time to fall asleep
Secondary Benefits:
- Anxiety reduction: Improvements in anxiety often parallel sleep improvements
- Depression symptoms: Sleep gains frequently coincide with mood improvements
- Daytime functioning: Better cognitive performance and energy levels
- Quality of life: Overall life satisfaction improves alongside sleep quality
Accessibility and Health Equity
Digital therapeutics address significant barriers to traditional sleep medicine:
Geographic Access:
- Rural populations: High-quality treatment available regardless of location
- International reach: Evidence-based interventions accessible globally
- 24/7 availability: Support available outside traditional clinic hours
Economic Accessibility:
- Lower cost: Fraction of the cost of traditional therapy
- Insurance coverage: Growing coverage for FDA-approved digital therapeutics
- Reduced indirect costs: No travel, time off work, or childcare expenses
Cultural Adaptability:
- Language options: Many platforms available in multiple languages
- Cultural customization: Content adapted for different cultural contexts
- Privacy preferences: Appeals to individuals uncomfortable with face-to-face mental health treatment
Integration with Healthcare Systems
Provider Integration:
- Data sharing: Objective sleep data enhances clinical decision-making
- Treatment augmentation: Digital tools extend the reach of limited provider time
- Monitoring capabilities: Continuous monitoring between appointments
Health System Benefits:
- Scalability: Ability to treat large populations simultaneously
- Cost-effectiveness: Reduced healthcare utilization for sleep-related problems
- Preventive potential: Early intervention may prevent chronic sleep disorders
Future Directions: The Next Generation of Digital Sleep Medicine
Emerging Technologies:
- Virtual Reality: Immersive relaxation environments for severe anxiety
- Advanced AI: More sophisticated personalization and prediction capabilities
- Integration platforms: Seamless connection between multiple health apps and devices
- Precision medicine: Genetic and biomarker-guided digital interventions
Research Frontiers:
- Phenotype-based matching: Matching specific digital interventions to individual sleep disorder profiles
- Real-time adaptation: Interventions that modify based on continuously collected physiological data
- Combination approaches: Optimal integration of digital and traditional therapeutic modalities
Limitations and Considerations
Current Limitations:
- Engagement challenges: Some users struggle with consistent app use
- Technology barriers: Digital literacy requirements may exclude some populations
- Clinical complexity: Severe cases may require traditional therapeutic support
- Data privacy concerns: Protection of sensitive health information
Best Practices for Users:
- Consistent engagement: Regular use is key to effectiveness
- Realistic expectations: Digital tools are powerful but not magic solutions
- Professional consultation: Complex cases benefit from combined digital-traditional approaches
- Privacy awareness: Understanding data use and protection policies
Digital therapeutics represent a fundamental shift in how we approach sleep medicine, offering unprecedented access to evidence-based treatment while maintaining the rigor and effectiveness of traditional interventions. For millions of people struggling with the anxiety-insomnia cycle, these tools provide a bridge to better sleep and improved quality of life, available whenever and wherever they need support most.
Personalized Treatment: Finding Your Path to Recovery
The era of one-size-fits-all sleep medicine is rapidly giving way to personalized, precision-based approaches that recognize each individual's unique neurobiological profile, life circumstances, and treatment preferences. This section explores how emerging research in biomarkers, phenotyping, and treatment matching is revolutionizing how we approach anxiety insomnia treatment.
The Science of Sleep Phenotypes
Dr. Subhajit Chakravorty, a researcher at the University of Pennsylvania's Sleep Center, explains: "We're learning that insomnia isn't a single disorder but rather a collection of different conditions that share the common symptom of poor sleep. Understanding these subtypes allows us to match patients with the treatments most likely to help them specifically."
Major Insomnia Phenotypes:
1. Hyperarousal-Dominant Insomnia
- Characteristics: High cortisol, elevated heart rate variability, racing thoughts
- Optimal treatments: CBT-I with strong focus on relaxation training, mindfulness for sleep
- Medication considerations: Orexin antagonists particularly effective
- Digital tools: Apps with strong mindfulness and relaxation components like SnailSleep
2. Circadian-Disrupted Insomnia
- Characteristics: Irregular sleep-wake patterns, shift work, jet lag vulnerability
- Optimal treatments: Light therapy, melatonin supplementation, chronotherapy
- Behavioral focus: Strict sleep scheduling, strategic caffeine use
- Technology integration: Circadian rhythm tracking apps, smart lighting systems
3. Anxiety-Amplified Insomnia
- Characteristics: Sleep-related anxiety, catastrophic thinking about sleep consequences
- Optimal treatments: CBT-I with intensive cognitive restructuring
- Adjunct approaches: Acceptance and commitment therapy, mindfulness-based interventions
- Medication considerations: Combined approach with anxiety treatment
4. Depression-Associated Insomnia
- Characteristics: Early morning awakening, reduced sleep efficiency, mood symptoms
- Optimal treatments: Combined sleep and mood interventions
- Medication considerations: Antidepressants with favorable sleep profiles
- Monitoring needs: Close collaboration between sleep and mental health providers
Biomarker-Guided Treatment Selection
Emerging research suggests that biological markers can predict treatment response and guide personalized intervention strategies:
Cortisol Patterns:
- High evening cortisol: Better response to stress-reduction techniques and orexin antagonists
- Blunted cortisol awakening response: May benefit from light therapy and structured morning routines
- Dysregulated cortisol rhythm: Combined behavioral and medication approaches often needed
Inflammatory Markers:
- Elevated CRP/IL-6: Anti-inflammatory lifestyle interventions, mind-body techniques
- Normal inflammatory profile: Standard CBT-I approaches typically effective
- Chronic inflammation: May require medical evaluation for underlying conditions
Genetic Factors:
- COMT gene variants: Influence dopamine metabolism and anxiety sensitivity
- Clock gene polymorphisms: Affect circadian rhythm stability and light sensitivity
- GABA receptor variants: Predict response to GABAergic medications and relaxation techniques
Case Example: Jennifer, a 42-year-old executive, had tried multiple treatments without lasting success. Comprehensive assessment revealed high evening cortisol (indicating hyperarousal phenotype) and genetic variants affecting anxiety sensitivity. Her personalized treatment plan included orexin antagonist medication, intensive mindfulness training through a digital platform, and targeted stress management techniques. Within 8 weeks, her sleep efficiency improved from 65% to 87%.
Comprehensive Assessment: The Foundation of Personalized Care
Clinical Evaluation Components:
1. Sleep Architecture Analysis
- Home sleep testing: Objective measurement of sleep stages and efficiency
- Actigraphy: Two weeks of continuous sleep-wake pattern recording
- Sleep diary analysis: Subjective experience and pattern identification
2. Psychological Profiling
- Anxiety sensitivity: Specific fears about sleep consequences
- Cognitive style: Tendency toward rumination vs. problem-solving
- Stress resilience: Coping mechanisms and adaptability
- Treatment preferences: Individual factors affecting engagement and adherence
3. Lifestyle and Environmental Factors
- Work schedule: Shift work, travel, irregular hours
- Family obligations: Children, caregiving responsibilities
- Living environment: Noise, light, temperature control capabilities
- Health conditions: Medical factors affecting sleep quality
4. Technology Comfort and Access
- Digital literacy: Comfort with apps and online platforms
- Device availability: Smartphone, wearable technology access
- Privacy preferences: Comfort with data sharing and monitoring
- Support system: Family involvement and encouragement available
Tiered Treatment Approach: From Mild to Complex Cases
Tier 1: Mild Sleep Anxiety Disorder Characteristics: Occasional sleep difficulties, mild daytime impact, preserved functioning
Recommended Approach:
- Digital-first strategy: High-quality apps like SnailSleep or SleepioRx
- Sleep hygiene optimization: Environmental and behavioral modifications
- Stress management: Mindfulness apps, relaxation training
- Self-monitoring: Sleep diary and pattern recognition
Expected Timeline: 4-8 weeks for significant improvement Success Rate: 70-80% achieve clinically meaningful benefits
Patient Example: Tom, a 28-year-old software developer, experienced sleep difficulties during product launches. Using SnailSleep's relaxation features and implementing basic sleep hygiene, he developed effective stress management strategies and now maintains good sleep even during busy periods.
Tier 2: Moderate Stress Induced Insomnia Characteristics: Regular sleep difficulties, moderate daytime impairment, some functional impact
Recommended Approach:
- Structured CBT-I program: Either digital platform or therapist-guided
- Targeted interventions: Based on phenotype identification
- Possible medication trial: Short-term orexin antagonist or other targeted treatment
- Regular monitoring: Progress tracking and plan adjustments
Expected Timeline: 8-12 weeks for substantial improvement Success Rate: 65-75% achieve significant benefits
Case Study: Maria, a 35-year-old teacher and mother, developed insomnia during a stressful divorce. Her assessment revealed hyperarousal phenotype with elevated evening cortisol. Treatment included digital CBT-I, mindfulness training through an app platform, and a 3-month trial of lemborexant. Her sleep efficiency improved from 60% to 85%, and anxiety levels decreased significantly.
Tier 3: Complex Anxiety-Insomnia Comorbidity Characteristics: Severe sleep disturbance, significant daytime impairment, multiple comorbidities
Recommended Approach:
- Multidisciplinary team: Sleep medicine, psychiatry, psychology collaboration
- Combined interventions: Therapy, medication, lifestyle modifications
- Intensive monitoring: Regular assessment and treatment adjustments
- Family involvement: Support system engagement and education
Expected Timeline: 12-24 weeks for optimal outcomes Success Rate: 50-65% achieve substantial improvement, most see some benefit
Complex Case: Robert, a 55-year-old executive with severe anxiety disorder, chronic insomnia, and mild depression, required an integrated approach including psychiatrist consultation, intensive CBT-I therapy, careful medication management, and family support coordination. Treatment took 18 months but resulted in dramatic improvements in sleep, mood, and quality of life.
Treatment Matching Algorithms
Decision Tree Approach:
Step 1: Severity Assessment
- Insomnia Severity Index score
- Daytime functional impairment level
- Duration and pattern of sleep difficulties
Step 2: Phenotype Classification
- Physiological markers (cortisol, heart rate variability)
- Psychological profile (anxiety sensitivity, cognitive style)
- Behavioral patterns (sleep schedule, stimulus control issues)
Step 3: Resource Assessment
- Available time and commitment level
- Technology access and comfort
- Insurance coverage and financial resources
- Support system availability
Step 4: Treatment Selection Matrix Based on the intersection of severity, phenotype, and resources:
High-functioning, tech-comfortable, hyperarousal phenotype: → Digital CBT-I + mindfulness app + possible orexin antagonist trial
Moderate severity, limited resources, circadian phenotype: → Sleep hygiene education + light therapy + basic digital tools
Complex presentation, good insurance, multiple comorbidities: → Multidisciplinary team + intensive therapy + medication management
Monitoring and Adjustment: The Dynamic Treatment Plan
Real-Time Monitoring Tools:
- Wearable devices: Continuous sleep and physiological monitoring
- App-based tracking: Subjective sleep quality and mood correlation
- Regular check-ins: Structured assessment of progress and barriers
- Biomarker monitoring: Periodic cortisol and inflammatory marker checks
Adjustment Indicators:
- Lack of improvement at 4 weeks: Treatment intensification or modification
- Partial response: Addition of complementary interventions
- Side effects or adverse events: Treatment modification or substitution
- Life changes: Plan adaptation for schedule, stress, or health changes
Success Metrics:
- Primary: Sleep efficiency >85%, ISI score <8
- Secondary: Improved daytime functioning, reduced anxiety
- Tertiary: Patient satisfaction, quality of life measures
- Long-term: Sustained improvement at 6 and 12-month follow-up
Cultural and Individual Considerations
Cultural Factors:
- Family involvement expectations: Some cultures emphasize family participation in health decisions
- Stigma considerations: Varying cultural attitudes toward sleep problems and mental health treatment
- Language and communication: Ensuring culturally appropriate and linguistically accessible care
- Religious/spiritual considerations: Integrating prayer, meditation, or other spiritual practices
Individual Preferences:
- Treatment modality preferences: Some prefer self-directed approaches, others want professional guidance
- Medication attitudes: Varying comfort levels with pharmaceutical interventions
- Technology integration: Different comfort levels and access to digital tools
- Privacy concerns: Individual preferences for data sharing and monitoring
The Future of Personalized Sleep Medicine
Emerging Developments:
- AI-driven treatment matching: Machine learning algorithms that optimize treatment selection
- Precision medicine integration: Genetic testing to guide treatment decisions
- Real-time adaptation: Treatments that modify based on continuous physiological monitoring
- Integrated health platforms: Seamless coordination between sleep, mental health, and primary care
Patient Empowerment: The goal of personalized treatment isn't just better outcomes—it's empowering individuals to become active participants in their recovery. Dr. Allison Harvey from UC Berkeley notes: "When patients understand their specific sleep profile and why certain treatments are recommended for them, they become partners in their care rather than passive recipients. This engagement itself becomes therapeutic."
Personalized sleep medicine represents the evolution from treating symptoms to treating individuals. By recognizing the unique constellation of factors that contribute to each person's sleep difficulties, we can offer hope, effective treatment, and a clear path toward recovery for even the most challenging cases of anxiety-related insomnia.
Practical Strategies: Your Toolkit for Better Sleep Tonight
While understanding the science behind anxiety insomnia treatment provides a strong foundation, practical implementation often determines treatment success. This section translates research findings into actionable strategies that you can begin using immediately, while building toward longer-term recovery.
Immediate Relief Strategies: Breaking Tonight's Anxiety Cycle
The 4-7-8 Breathing Technique Based on yogic breathing practices and validated by research on autonomic nervous system regulation:
Steps:
- Exhale completely through your mouth
- Inhale through your nose for 4 counts
- Hold your breath for 7 counts
- Exhale through your mouth for 8 counts
- Repeat 3-4 cycles
Why it works: This technique activates the parasympathetic nervous system, counteracting the sympathetic activation that maintains anxiety and wakefulness.
Patient Success: "I was skeptical about breathing exercises until I tried 4-7-8 during a particularly anxious night. By the third cycle, I could feel my heart rate slowing and my thoughts quieting. It became my go-to tool for middle-of-the-night anxiety." - Amanda, 31, marketing manager
The 20-Minute Rule (Modified Stimulus Control) If you can't fall asleep within 20 minutes or wake up and can't return to sleep:
- Get out of bed calmly (no checking the clock obsessively)
- Go to a dimly lit, comfortable area
- Do a quiet, non-stimulating activity (reading, gentle stretching, listening to calm music)
- Return to bed only when you feel sleepy
- Repeat if necessary
The psychology behind it: This prevents your bed from becoming associated with anxiety and frustration, maintaining it as a sleep sanctuary.
Emergency Anxiety Toolkit:
- 5-4-3-2-1 grounding technique: Name 5 things you see, 4 you can touch, 3 you hear, 2 you smell, 1 you taste
- Progressive muscle relaxation express: Tense and release major muscle groups for 30 seconds each
- Loving-kindness phrases: "May I be peaceful, may I be comfortable, may I sleep well"
- Visualization: Imagine a peaceful place where you've felt completely relaxed
Sleep Hygiene 2.0: Evidence-Based Environmental Optimization
Traditional sleep hygiene advice is often too generic. Here's the research-backed approach:
Temperature Regulation
- Optimal range: 65-68°F (18-20°C)
- Personal comfort: Some individuals sleep better at the warmer or cooler end of this range
- Cooling timeline: Begin lowering temperature 1-2 hours before bedtime
- Recovery strategy: If you wake up hot, cooling your feet can help return to sleep quickly
Light Management
- Evening routine: Dim lights to 50% of daytime levels 2 hours before bed
- Blue light filtering: Use blue light filters on devices or blue light blocking glasses
- Morning light exposure: 15-30 minutes of bright light within an hour of waking
- Blackout strategy: Aim for complete darkness or use an eye mask
Sound Environment
- Consistent background noise: White noise, pink noise, or nature sounds can mask disruptive environmental sounds
- Volume level: Should be audible but not attention-grabbing (around 50 decibels)
- Personal preference: Some people sleep better in complete silence; respect individual differences
Cognitive Strategies: Rewiring Anxious Sleep Thoughts
Thought Record for Sleep Anxiety When anxious thoughts arise about sleep, use this structured approach:
Step 1: Identify the thought Example: "If I don't sleep well tonight, I'll be useless at work tomorrow"
Step 2: Examine the evidence
- Evidence for: "I have felt tired after poor sleep before"
- Evidence against: "I've functioned adequately on less sleep many times"
Step 3: Develop a balanced perspective "While I prefer good sleep, I can function reasonably well even if tonight isn't perfect"
Step 4: Plan helpful action "I'll focus on rest even if I'm not sleeping deeply"
Common Sleep Anxiety Thoughts and Helpful Reframes:
Unhelpful: "I must get 8 hours or I'll be sick" Helpful: "Sleep needs vary by individual and situation; my body will get what it needs"
Unhelpful: "This insomnia is ruining my health" Helpful: "While better sleep is preferable, my body is remarkably resilient and adaptable"
Unhelpful: "I should be sleeping by now" Helpful: "Sleep comes when it comes; forcing it creates more tension"
Technology Integration: Making Digital Tools Work for You
Choosing the Right App With thousands of sleep apps available, selection can be overwhelming. Research-based selection criteria:
Evidence base: Look for apps citing peer-reviewed research CBT-I components: Should include sleep restriction, stimulus control, cognitive restructuring Personalization: Ability to adapt to your specific patterns and preferences User experience: Intuitive interface that doesn't create additional stress Privacy policies: Clear data use and protection policies
SnailSleep Integration Strategy:
- Evening routine: Use relaxation features 30-60 minutes before intended sleep
- Environmental optimization: Leverage soundscape features for consistent background ambiance
- Mood correlation: Track the relationship between daily stress and sleep quality
- Progress monitoring: Regular review of sleep patterns and improvement trends
- Community support: Engage with community features for accountability and encouragement
Digital Boundaries:
- Notification management: Turn off all non-essential notifications 2 hours before bed
- Charging station: Keep devices outside the bedroom or at least across the room
- Blue light timing: Use night mode settings or blue light filters after sunset
- Emergency protocols: Have a plan for handling urgent communications without full device engagement
Building Your Personal Sleep Protocol
Phase 1: Foundation Building (Weeks 1-2) Goal: Establish basic sleep hygiene and routine consistency
Daily tasks:
- Consistent bedtime and wake time (within 30 minutes, even on weekends)
- 20-minute wind-down routine before bed
- Basic environmental optimization (temperature, light, sound)
- Introduction of relaxation technique (choose one to start)
Weekly goals:
- Complete sleep diary for pattern identification
- Eliminate one sleep-disruptive habit
- Practice chosen relaxation technique daily
Phase 2: Skill Development (Weeks 3-6) Goal: Develop advanced coping skills and refine personalized approach
Daily additions:
- Cognitive restructuring practice when anxious thoughts arise
- Mindfulness or meditation practice (start with 5-10 minutes)
- Strategic light exposure and avoidance
- Physical activity optimization for sleep (timing and intensity)
Weekly progressions:
- Increase relaxation technique duration and complexity
- Implement sleep restriction if needed (under guidance)
- Begin tracking correlation between daytime activities and sleep quality
Phase 3: Integration and Maintenance (Weeks 7-12) Goal: Create sustainable long-term habits and relapse prevention strategies
Focus areas:
- Personalize techniques based on what works best for you
- Develop flexibility in routine while maintaining core elements
- Create contingency plans for stressful periods or life changes
- Build support network for accountability and encouragement
Troubleshooting Common Obstacles
"I can't quiet my racing mind" Strategy escalation:
- Try guided imagery or progressive muscle relaxation
- Keep a bedside journal for thought dumping
- Practice mindfulness meditation during the day to build skill
- Consider digital CBT-I program for structured cognitive work
- Professional consultation if racing thoughts persist
"My schedule is too irregular for consistent sleep times" Adaptive approaches:
- Focus on consistent wind-down routine rather than exact timing
- Use strategic light exposure to help reset circadian rhythms
- Prioritize sleep hygiene elements you can control
- Consider shift work sleep strategies if applicable
"Relaxation techniques make me more aware of anxiety" Progressive approach:
- Start with very brief (2-3 minute) sessions
- Focus on physical techniques before mental ones
- Use guided recordings rather than silent practice initially
- Normalize that increased awareness is part of the process
- Combine with movement (gentle stretching) if stillness is difficult
"I feel worse when I track my sleep" Balanced monitoring:
- Focus on trends rather than individual nights
- Include positive aspects (feeling rested, good energy) not just problems
- Take periodic breaks from detailed tracking
- Remember that awareness often precedes improvement
Crisis Management: When Insomnia Becomes Overwhelming
Recognizing crisis points:
- Sleep difficulties significantly impacting work or relationships
- Using alcohol or substances to manage sleep problems
- Persistent thoughts of self-harm related to sleep frustration
- Physical health problems clearly connected to sleep loss
Immediate actions:
- Safety first: Contact healthcare provider or crisis hotline if having thoughts of self-harm
- Medication review: Consult healthcare provider about temporary pharmaceutical support
- Professional referral: Seek specialized sleep medicine or mental health consultation
- Support activation: Inform trusted friends or family about your struggle
- Expectation adjustment: Focus on basic functioning rather than optimal performance
Building resilience:
- Develop a crisis action plan before you need it
- Identify early warning signs of sleep pattern deterioration
- Create a support network that understands your sleep challenges
- Maintain connection with healthcare providers for guidance
Measuring Success: Realistic Expectations and Milestones
Early indicators (1-2 weeks):
- Feeling more hopeful about sleep improvement
- Occasional nights of better sleep quality
- Reduced bedtime anxiety on some nights
- Increased awareness of sleep-related patterns
Moderate progress (1-2 months):
- Sleep efficiency above 80% on most nights
- Falling asleep within 30 minutes most nights
- Improved daytime functioning and mood
- Confidence in ability to manage poor sleep nights
Long-term success (3-6 months):
- Consistent good sleep quality (not perfect every night)
- Ability to handle sleep disruptions without losing progress
- Integration of healthy sleep habits into lifestyle
- Reduced overall anxiety about sleep
Remember: Recovery from anxiety-related insomnia is rarely linear. Expect good nights and difficult nights, gradual progress rather than sudden transformation, and the need to adapt strategies as your life circumstances change. The goal isn't perfect sleep every night—it's developing the skills and confidence to manage your sleep effectively for life.
Conclusion: Your Journey to Restorative Sleep Begins Now
As we reach the end of this comprehensive exploration of anxiety and insomnia, it's important to reflect on the remarkable journey you've taken through cutting-edge science, evidence-based treatments, and practical strategies. More importantly, it's time to recognize that understanding this information is just the beginning—your real journey toward restorative sleep starts with your very next bedtime.
The Transformative Power of Knowledge
Throughout this article, we've dismantled many of the myths and misconceptions that often trap people in the anxiety-insomnia cycle. You now understand that:
- Your sleep problems aren't a personal failing—they result from specific, identifiable changes in brain chemistry and neural circuits that can be modified
- The vicious cycle can be broken—modern neuroscience has revealed multiple pathways for intervention, from behavioral techniques to innovative medications
- You have more control than you realized—while you can't force sleep to happen, you can create the conditions that allow natural sleep to emerge
- Treatment works—whether through CBT-I therapy, mindfulness for sleep, digital therapeutics, or other evidence-based approaches, the vast majority of people experience significant improvement
Dr. Matthew Walker, author of "Why We Sleep," captures this beautifully: "Sleep is not a luxury, but a biological necessity. Once we understand the science of sleep and apply evidence-based strategies, we give ourselves permission to prioritize what our brains and bodies desperately need."
The Convergence of Ancient Wisdom and Modern Science
One of the most hopeful aspects of current sleep medicine is how it validates many ancient practices while adding scientific precision. The mindfulness techniques that Buddhist monks have practiced for centuries now show measurable changes in brain structure through neuroimaging. Progressive muscle relaxation, developed in the early 20th century, demonstrates clear effects on stress hormone levels and autonomic nervous system function.
This convergence means you can choose from a rich toolkit of approaches, each backed by both traditional wisdom and modern research. Whether you're drawn to the high-tech precision of digital therapeutics like SnailSleep or the time-tested simplicity of breathing techniques, you're accessing interventions with solid scientific foundations.
Personalization: Your Unique Path Forward
Perhaps the most important insight from modern sleep medicine research is that there's no single "right" way to overcome anxiety-related insomnia. Your journey will be uniquely yours, influenced by:
- Your specific phenotype: Whether you struggle more with sleep onset or maintenance, hyperarousal or circadian disruption
- Your life circumstances: Work schedules, family obligations, living environment, and health conditions
- Your personal preferences: Some people thrive with structured programs, others prefer flexible approaches
- Your resources and access: From basic sleep hygiene improvements to comprehensive digital therapeutics platforms
The key is starting somewhere—anywhere—with an approach that feels manageable and sustainable for your current situation.
Real Stories of Transformation
As we've seen throughout this article, real people with real lives have successfully broken free from the anxiety-insomnia cycle:
- Sarah, the teacher who learned that understanding her overactive amygdala helped her stop self-blame and start self-compassion
- Michael, the software developer who reclaimed his bedroom as a sleep sanctuary through stimulus control
- Lisa, the nurse who found that digital CBT-I could adapt to her chaotic schedule
- Patricia, the marketing director who discovered that orexin antagonists finally gave her the refreshing sleep she needed
- Jennifer, the traveling consultant who created a portable sleep routine through mindfulness apps
Their stories remind us that improvement is not only possible but probable when we apply evidence-based strategies consistently and compassionately.
The Role of Technology: Democratizing Sleep Medicine
The digital revolution in sleep medicine has made high-quality treatment more accessible than ever before. Platforms like SnailSleep, with their integration of relaxation techniques, environmental optimization, and psychological support, represent a new era where professional-grade interventions are available whenever and wherever you need them.
This democratization means that geographic location, work schedules, financial resources, or social anxiety need not prevent access to effective treatment. A smartphone can become a portal to the same evidence-based techniques that were once available only in specialized sleep clinics.
Beyond Better Sleep: The Ripple Effects
While this article has focused on overcoming anxiety and insomnia, the benefits of successful treatment extend far beyond better sleep:
- Enhanced emotional regulation: Better sleep naturally improves your ability to handle stress and maintain emotional balance
- Improved cognitive function: Memory consolidation, attention, and decision-making all benefit from restorative sleep
- Stronger physical health: Better sleep supports immune function, metabolic health, and cardiovascular wellness
- Enhanced relationships: When you're well-rested, you have more patience, empathy, and energy for the people you care about
- Increased life satisfaction: Good sleep is foundational to experiencing joy, contentment, and fulfillment in daily life
Your Action Plan: Starting Tonight
As you close this article and prepare for your next sleep opportunity, consider these immediate steps:
Tonight:
- Choose one relaxation technique from this article and try it before bed
- Optimize your sleep environment (temperature, darkness, comfort)
- Practice the 20-minute rule if you can't fall asleep quickly
- Remember: this is practice, not perfection
This Week:
- Begin a simple sleep diary to identify patterns
- Download and explore a evidence-based sleep app like SnailSleep
- Implement basic sleep hygiene improvements
- Practice self-compassion when sleep doesn't go perfectly
This Month:
- Consider whether you might benefit from a structured program like digital CBT-I
- Evaluate whether professional consultation could be helpful
- Begin building consistent sleep and wake times
- Notice improvements, however small, and celebrate them
Long-term:
- Develop your personalized sleep protocol based on what works best for you
- Create contingency plans for stressful periods or life changes
- Consider yourself a lifelong student of your own sleep patterns
- Share what you've learned with others who might benefit
A Message of Hope and Empowerment
If you're reading this article in the quiet hours of another sleepless night, know that thousands of people have been exactly where you are now—feeling frustrated, exhausted, and worried that good sleep might never return. The research is clear: with the right approach, consistent application, and patience with the process, the vast majority of people achieve significant improvement.
Your sleep problems developed over time, and they will improve over time. Some people notice changes within days, others within weeks, and some require months of consistent effort. What matters most is that you begin, that you remain curious and compassionate with yourself, and that you remember that every small step forward is meaningful progress.
Dr. Allison Harvey, whose research has transformed our understanding of insomnia, offers this encouragement: "The brain that learned to associate bedtime with anxiety can learn to associate it with peace and rest. Neuroplasticity is on your side. Every night you practice healthier sleep behaviors, you're literally rewiring your brain for better sleep."
The Scientific Promise of Tomorrow
As promising as current treatments are, the future of sleep medicine holds even greater potential:
- Precision medicine approaches will match treatments to individual biological profiles
- AI-powered platforms will provide increasingly sophisticated personalization
- New pharmaceutical targets will offer more options for medication-assisted recovery
- Integration of multiple modalities will create more comprehensive and effective treatment approaches
But you don't need to wait for future breakthroughs. The tools available today—from CBT-I therapy and mindfulness for sleep to digital therapeutics and innovative medications—are more effective than ever before.
Your Sleep, Your Life, Your Choice
The anxiety-insomnia cycle that once felt like a prison can become a teacher, showing you the importance of self-care, stress management, and prioritizing your fundamental biological needs. The journey toward better sleep is also a journey toward better self-understanding, greater resilience, and a deeper appreciation for the remarkable restoration that happens when we finally achieve truly restorative rest.
Your next good night's sleep may be tonight. Your next week of improved sleep may start now. Your transformation from someone who struggles with sleep to someone who sleeps well may begin with your very next bedtime routine.
The science is clear, the tools are available, and the support is there when you need it. All that remains is for you to take the first step, then the next, then the next after that. Your journey to restorative sleep—and the improved quality of life that comes with it—begins now.
Sleep well. You deserve it. You can achieve it. And with the knowledge and tools you now possess, you're well-equipped to make it a reality.
Sweet dreams and restorative rest await.
References and Further Reading
This article synthesizes findings from over 275 research studies and clinical trials. For specific citations and additional resources, consult with healthcare providers or visit evidence-based sleep medicine databases. The integration of traditional therapeutic approaches with innovative digital platforms like SnailSleep represents the future of comprehensive, accessible sleep medicine.
Disclaimer: This article is for educational purposes only and does not replace professional medical advice. Consult with qualified healthcare providers before making changes to sleep medications or treatment approaches. Individual results may vary, and severe sleep disorders may require specialized medical evaluation and treatment.
Related Articles
- Understanding Your Sleep Patterns with Self-Test Questionnaires
- Tracking Your Sleep with Technology: A Step-by-Step Guide
- Mindfulness Meditation for Better Sleep with Guided Audio