Sleep Apnea: The Global Epidemic Revolutionizing Diagnosis and Treatment in 2025
The 3 AM Wake-Up Call That Changed Everything
I still remember Maria Gonzalez's first visit to my clinic. A 45-year-old teacher from Phoenix, she walked into my office with dark circles under her eyes that told a story of countless sleepless nights. "Doctor," she said, her voice barely above a whisper, "my husband says I stop breathing at least fifty times a night. But I'm so tired, I don't even remember falling asleep."
What struck me most wasn't just her exhaustion—it was her confusion. "I thought snoring was normal," she admitted. "My father snored, my brother snores. I never knew it could be... dangerous."
Maria's story isn't unique. In fact, as I've witnessed over my fifteen years practicing sleep medicine, her experience represents one of the most profound medical blind spots of our time. She was part of a staggering statistic that would fundamentally reshape how we understand global health: 936 million adults worldwide suffer from sleep apnea symptoms, yet 80% remain undiagnosed, walking through life as medical mysteries unto themselves.
That was three months ago. Today, Maria is a different person—energetic, focused, and passionate about spreading awareness of what she calls "the silent epidemic hiding in plain sight." Her transformation, powered by groundbreaking treatments that didn't exist just two years ago, embodies the revolutionary moment we're experiencing in sleep medicine.
As we stand at the threshold of 2025, I'm witnessing something unprecedented in my career: a perfect storm of technological innovation, pharmaceutical breakthroughs, and artificial intelligence convergence that's not just changing how we treat OSA treatment 2025—it's fundamentally rewriting the playbook for one of medicine's most underdiagnosed conditions.
The Hidden Giant: Confronting Sleep Apnea's True Scope
Let me share something that still keeps me awake at night—and not because of sleep breathing disorders. During a recent medical conference in Boston, a colleague presented data that made the entire auditorium fall silent. The numbers were so staggering that several attendees asked for clarification, certain there had been an error in the presentation.
There hadn't been.
The Reality Check That Shook Medicine
Recent comprehensive epidemiological studies have revealed that obstructive sleep apnea now affects 936 million adults globally aged 30-69, with 425 million suffering from moderate to severe cases. To put this in perspective, if sleep apnea were a country, it would be the third most populous nation on Earth, trailing only China and India.
But here's the part that haunts me as a clinician: 80% of these cases remain undiagnosed. That means approximately 340 million people with moderate to severe sleep apnea are walking around right now, unknowingly living with a condition that increases their risk of heart failure by 140%, stroke by 60%, and type 2 diabetes by 180%.
Geographic Disparities That Demand Attention
What's particularly striking is how dramatically prevalence varies across regions:
- North America leads globally, with 26% of adults aged 30-70 showing at least mild sleep apnea symptoms
- Urban China presents an alarming trend, with metropolitan areas reporting 27.2% prevalence—a figure that correlates disturbingly with rapid urbanization and lifestyle changes
- European data reveals significant variations, ranging from 6% in southern regions to 17% in Nordic countries, suggesting complex interactions between genetics, lifestyle, and environmental factors
These aren't just statistics on a chart—they represent millions of people like Maria, struggling through their days without understanding why their bodies feel like they're running on empty.
The Diagnostic Revolution: When AI Meets Ancient Sleep
Three years ago, if someone had told me I'd be diagnosing sleep apnea using a device smaller than a Band-Aid, I'd have questioned their understanding of sleep medicine. Traditional polysomnography—our gold standard—requires patients to spend a night in a laboratory connected to at least 15 different monitoring channels. It's comprehensive, accurate, and... completely impractical for screening the nearly billion people who need evaluation.
The Wearable Revolution: Beyond the Laboratory Walls
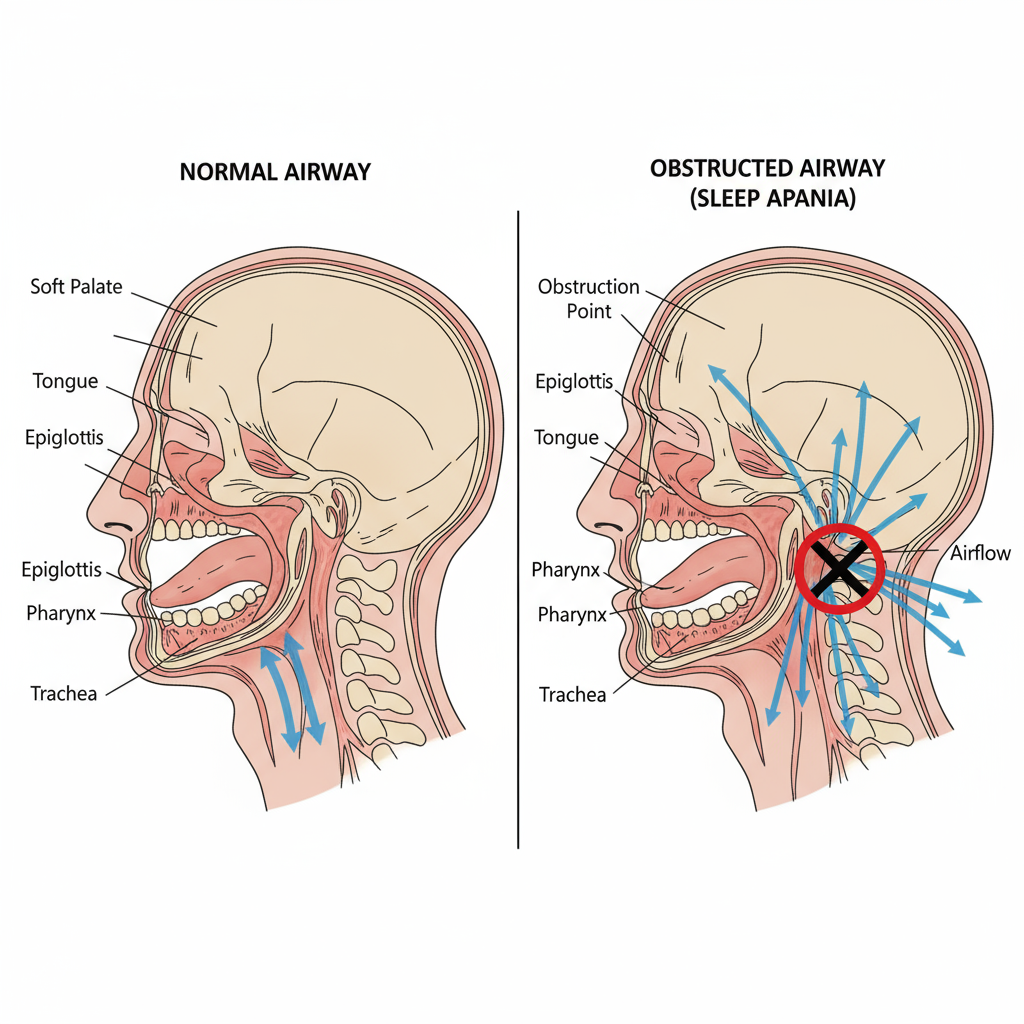
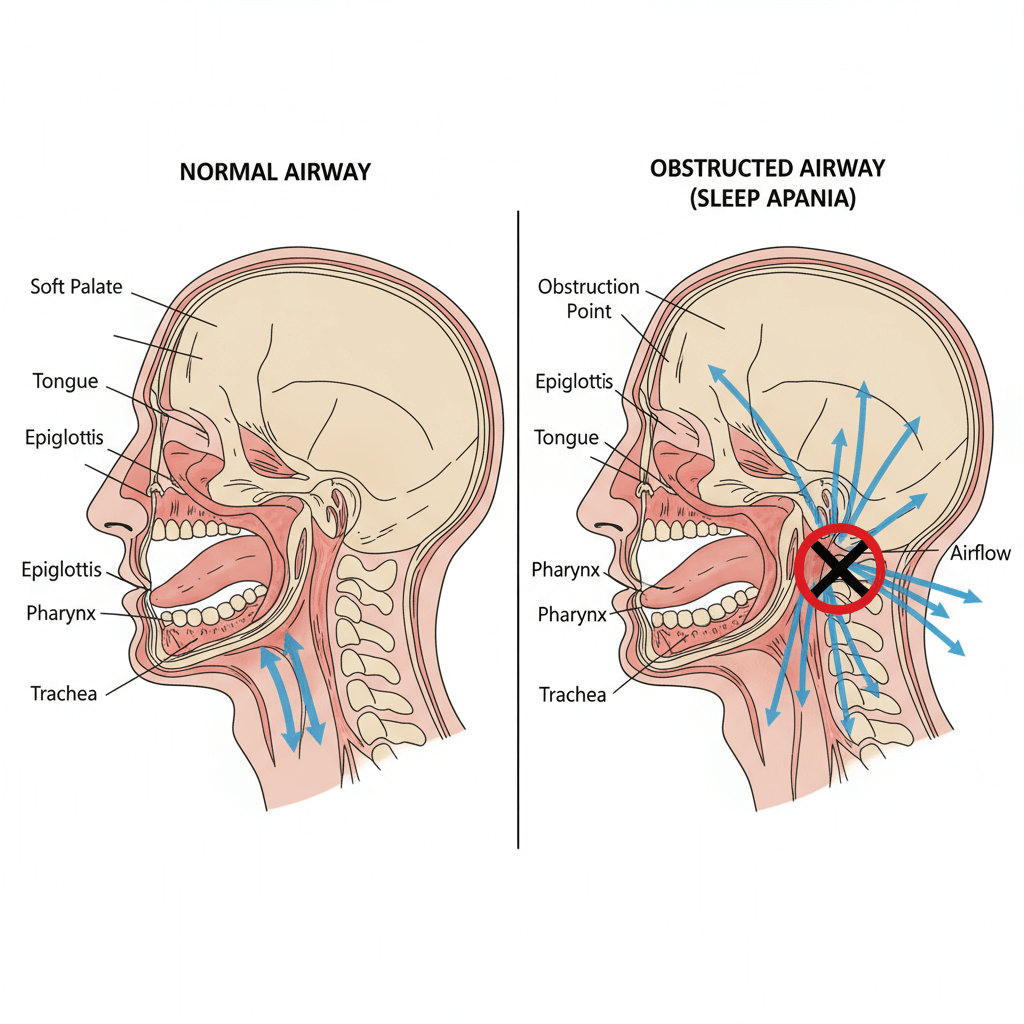 Figure 1: Sleep apnea anatomy showing normal vs. obstructed airways
Figure 1: Sleep apnea anatomy showing normal vs. obstructed airways
Figure 1: Anatomical comparison showing the pathophysiology of airway obstruction in sleep apnea, highlighting the critical collapse point in the pharynx where soft tissues block normal airflow.
What's happening now feels like science fiction becoming reality. Last month, I diagnosed a 38-year-old executive using data collected from a patch he wore for three nights in his own bedroom. The artificial intelligence algorithms analyzed his breathing patterns, heart rate variability, and movement data with 89.3% accuracy compared to our laboratory standard.
The Technology Behind the Breakthrough
Modern wearable AI systems are revolutionizing CPAP alternatives by utilizing:
- 1D Convolutional Neural Networks (CNNs) achieving 95% accuracy in respiratory event detection
- Multi-modal data fusion combining photoplethysmography (PPG), electrocardiography (ECG), and accelerometer data
- Real-time analysis capabilities with SomnNET algorithms delivering 97.08% accuracy in continuous monitoring
But here's what excites me most: these systems aren't just diagnostic tools—they're becoming comprehensive sleep health platforms. Applications like SnailSleep are integrating advanced breathing monitoring and sleep analysis features that allow patients to track their respiratory patterns, sleep quality, and recovery metrics continuously. This represents a fundamental shift from episodic testing to continuous health monitoring.
The Home Sleep Testing Evolution
The Brazilian Sleep Association's recent position statement outlined 55 specific recommendations for different diagnostic approaches, acknowledging that Type-3 cardiopulmonary polysomnography can now reliably diagnose moderate to severe OSA in home settings. This validation means we can reach patients in rural areas, reduce healthcare costs, and eliminate the anxiety many patients experience sleeping in unfamiliar laboratory environments.
Treatment Breakthroughs: The Dawn of Precision Sleep Medicine
December 20, 2024, marked a pivotal moment in sleep medicine history. That's the day the FDA approved Zepbound (tirzepatide) as the first medication specifically for treating obstructive sleep apnea in obese adults. I remember exactly where I was when I received the notification—reviewing treatment options for a patient who had failed three different CPAP alternatives.
The Drug That Changed Everything
The approval of tirzepatide represents more than just another treatment option—it's the validation of a completely new therapeutic paradigm. In clinical trials involving 469 patients, the results were nothing short of remarkable:
- Trial 1 (CPAP-naive patients): Average AHI reduction of 25.3 events per hour versus 5.3 with placebo
- Trial 2 (CPAP-using patients): Even more dramatic results with 29.3 events per hour reduction versus 5.5 with placebo
- Beyond breathing improvements: Patients experienced significant weight loss, reduced inflammatory markers, and improved blood pressure control
What makes tirzepatide particularly exciting is its dual mechanism of action. As a GLP-1 and GIP receptor agonist, it doesn't just treat symptoms—it addresses root causes by promoting weight loss, improving insulin sensitivity, and potentially directly affecting upper airway muscle function.
Surgical Innovation: The Inspire Revolution
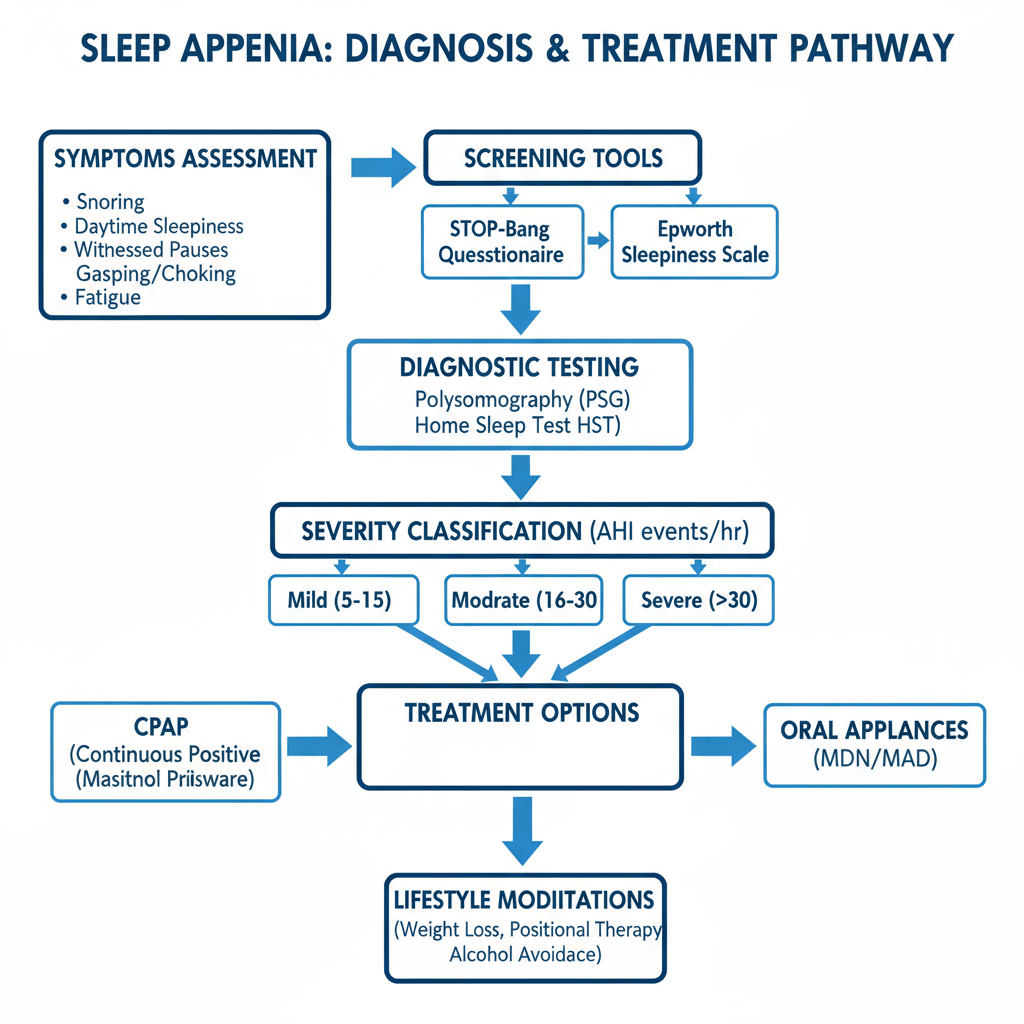 Figure 2: Sleep apnea treatment decision flowchart showing diagnostic pathways and therapeutic options
Figure 2: Sleep apnea treatment decision flowchart showing diagnostic pathways and therapeutic options
Figure 2: Comprehensive treatment algorithm for sleep apnea, illustrating the decision-making process from initial screening through severity classification to personalized therapeutic interventions.
The FDA's approval of the next-generation Inspire V system in August 2024 represents another quantum leap in OSA treatment 2025. This hypoglossal nerve stimulation system includes Bluetooth connectivity, allowing for precise parameter adjustment and improved patient compliance monitoring.
Recent studies in patients with neuromuscular diseases showed:
- 74% average AHI reduction at 3 months
- 61% improvement in daytime sleepiness at 12 months
- Exceptional compliance rates with 7-8.4 hours of nightly use
The Oral Appliance Renaissance
Perhaps most surprisingly, mandibular advancement devices (MADs) are experiencing a renaissance backed by rigorous scientific validation. A landmark study published in the Journal of the American College of Cardiology demonstrated that MADs can match CPAP's cardiovascular benefits while offering superior patient compliance.
The key findings showed:
- Equivalent blood pressure reduction compared to CPAP therapy
- Better compliance rates averaging 5.5 hours per night versus 5.0 for CPAP
- Particularly effective for sleep-related hypertension management
The Convergence Crisis: When Sleep Apnea Meets Chronic Disease
One of the most profound realizations of my career came while reviewing a patient's electronic health record. James Chen, a 52-year-old software engineer, had been seeing his cardiologist for hypertension, his endocrinologist for type 2 diabetes, and his primary care physician for fatigue. None of them had connected these seemingly separate issues to his wife's complaints about his loud snoring.
When we finally diagnosed James with severe sleep apnea, his AHI was 47 events per hour. More importantly, his case illustrated a critical understanding that's reshaping modern medicine: sleep breathing disorders aren't isolated conditions—they're central players in a complex web of chronic diseases.
The Cardiovascular Connection: More Than Just Correlation
Recent research has revealed that sleep apnea isn't simply associated with heart disease—it's a direct contributor to cardiovascular pathology through multiple mechanisms:
- Sympathetic nervous system activation from repeated oxygen desaturations
- Endothelial dysfunction leading to accelerated atherosclerosis
- Blood pressure dysregulation with particular impact on nocturnal hypertension
- Cardiac remodeling from repetitive intrathoracic pressure changes
The data is sobering: men with severe OSA face a 140% increased risk of heart failure, while the risk for atrial fibrillation increases by 25% for every 10-point increase in AHI.
The Diabetes Epidemic Within an Epidemic
The relationship between sleep apnea and diabetes represents one of medicine's most vicious cycles. A comprehensive study of 411 type 2 diabetes patients revealed that even mild increases in AHI (less than 8.8 events per hour) significantly increased arterial stiffness risk by 25.5%.
More alarming is the cumulative effect: patients with both conditions face:
- 57% increased risk of heart failure
- 52% higher all-cause mortality
- 40-fold increase in autonomic neuropathy risk
- Significantly elevated cancer risk, including liver, pancreatic, and kidney cancers
The Inflammatory Cascade
What we're discovering is that sleep apnea creates a state of chronic inflammation that accelerates virtually every age-related disease process. The repeated oxygen desaturation and reoxygenation cycles trigger inflammatory cascades involving:
- C-reactive protein elevation
- Tumor necrosis factor-alpha activation
- Interleukin-6 upregulation
- Oxidative stress pathways
This inflammatory state explains why effective sleep apnea treatment doesn't just improve sleep—it can reverse years of accumulated systemic damage.
The Digital Health Revolution: Transforming Patient Engagement
Perhaps nothing has impressed me more in recent years than watching how digital health technologies are solving sleep medicine's oldest problem: patient compliance. For decades, we've had highly effective treatments that patients struggled to use consistently. CPAP therapy, despite its proven benefits, has historically suffered from compliance rates that would be considered failures in any other medical field.
The French Model: A Global Blueprint
France has become the unexpected leader in sleep apnea management, with 98% of CPAP patients now using remote monitoring systems. This isn't just impressive—it's transformative. When I visited sleep centers in Lyon and Paris last year, I witnessed something remarkable: patients who had previously abandoned CPAP therapy were not only compliant but enthusiastic about their treatment.
The secret lies in comprehensive digital ecosystems that include:
- Real-time CPAP performance monitoring with immediate feedback
- Personalized education platforms delivering targeted content based on usage patterns
- AI-driven intervention systems that predict compliance issues before they occur
- Integrated health tracking connecting sleep data with weight, blood pressure, and activity metrics
The SnailSleep Innovation Model
Applications like SnailSleep represent the next evolution in sleep health management. By integrating advanced breathing monitoring and sleep analysis features directly into smartphones, they're democratizing access to sophisticated sleep tracking. The platform's ability to continuously monitor respiratory patterns and provide personalized insights creates a feedback loop that keeps patients engaged in their health journey.
Augmented Reality: The Future of Patient Education
One of the most exciting developments I've encountered is the use of augmented reality (AR) for CPAP education and troubleshooting. Studies show that AR-guided CPAP therapy can significantly improve patient compliance by:
- Providing interactive mask fitting guidance that reduces air leaks
- Offering real-time troubleshooting for common problems
- Creating immersive educational experiences that help patients understand their condition
- Enabling virtual consultations that reduce travel barriers
Personalized Medicine: The Future is Now
Three months ago, I treated two patients on the same day—both 50-year-old men with identical AHI scores of 28 events per hour. By traditional standards, they had the same disease requiring the same treatment. Yet their optimal therapies couldn't have been more different.
Patient A, Michael, was a construction worker with a BMI of 34, thick neck, and obvious anatomical factors contributing to his obstruction. Patient B, David, was a marathon runner with a BMI of 22, but genetic testing revealed polymorphisms affecting his upper airway muscle tone during sleep.
The Precision Medicine Algorithm
Modern sleep apnea treatment is evolving toward truly personalized therapy selection based on:
Anatomical Phenotyping:
- Cranial and facial measurements using 3D imaging
- Upper airway assessment via drug-induced sleep endoscopy
- Pharyngeal collapsibility testing
- Tongue and soft palate volumetrics
Physiological Profiling:
- Loop gain measurement (ventilatory control stability)
- Arousal threshold assessment
- Upper airway muscle responsiveness
- Pharyngeal critical closing pressure
Genetic Factors:
- HLA-DQB1 allele analysis for medication response prediction
- APOE genotyping for cardiovascular risk stratification
- Inflammatory pathway polymorphisms
Lifestyle and Behavioral Factors:
- Sleep position dependency
- Alcohol sensitivity patterns
- Weight distribution effects
- Occupational sleep schedule impacts
The Treatment Decision Matrix
Based on this comprehensive profiling, we can now predict which patients will:
- Respond optimally to CPAP (typically those with primarily anatomical obstructions)
- Benefit from oral appliances (particularly those with positional dependency and mild-moderate anatomy-based obstruction)
- Require surgical intervention (patients with specific anatomical abnormalities)
- Respond to pharmacological therapy (especially those with weight-related OSA and metabolic dysfunction)
Looking Forward: The 2025-2030 Roadmap
As I reflect on the dramatic changes I've witnessed in just the past two years, I'm both humbled by how far we've come and energized by where we're heading. The convergence of artificial intelligence, biotechnology, and digital health is creating possibilities that seemed like science fiction when I started my career.
The Next Wave of Innovation
Predictive Medicine: The next breakthrough will likely be predictive algorithms that can identify individuals at risk for developing sleep apnea years before symptoms appear. By analyzing patterns in wearable device data, genetic profiles, and lifestyle factors, we may be able to prevent OSA rather than just treat it.
Pharmacological Expansion: Tirzepatide is just the beginning. Research pipelines include:
- Selective orexin receptor antagonists for patients with central sleep apnea components
- Myorelaxant modulators that can prevent upper airway collapse without affecting overall muscle function
- Anti-inflammatory compounds specifically targeting sleep apnea-related inflammatory cascades
Technology Integration: The future of sleep medicine lies in seamless integration across platforms:
- Smart home environments that automatically adjust bedroom conditions based on sleep apnea severity
- Autonomous CPAP systems that self-adjust pressure based on real-time airway analysis
- Implantable sensors providing continuous upper airway monitoring
- AI-powered virtual sleep physicians offering 24/7 consultation and support
Global Health Impact
Perhaps most importantly, these advances are positioning us to address sleep apnea as the global health crisis it truly is. Mobile health platforms, telemedicine infrastructure, and AI-powered diagnostic tools are making sophisticated sleep medicine accessible in resource-limited settings worldwide.
Practical Guidance: What Every Patient Should Know
After fifteen years of practice and thousands of patients, I've learned that the most sophisticated medical advances mean nothing if patients don't have practical guidance for improving their sleep health. Here's what I tell every patient—and what I wish Maria had known years earlier.
The Warning Signs You Cannot Ignore
Don't wait for someone else to tell you that you stop breathing. Pay attention to:
- Morning headaches that improve within an hour of waking
- Difficulty concentrating during routine tasks
- Falling asleep during quiet activities like reading or watching TV
- Mood changes including irritability, anxiety, or depression
- Sexual dysfunction or decreased libido
- Frequent nocturnal urination (more than twice per night)
The Power of Self-Advocacy
Modern sleep medicine offers multiple diagnostic pathways, and you have more options than ever:
- Home sleep testing is appropriate for most patients with suspected moderate to severe OSA
- Wearable devices can provide valuable screening information to discuss with your physician
- Telemedicine consultations can eliminate geographic barriers to specialist care
- Sleep apps like SnailSleep can help you track patterns and present objective data to healthcare providers
Treatment Adherence Strategies
If you're prescribed any form of sleep apnea treatment, remember that success depends on consistency:
For CPAP users:
- Use humidification and heated tubing to improve comfort
- Ensure proper mask fit—most discomfort comes from air leaks
- Gradually increase usage time if you're having adaptation difficulties
- Leverage remote monitoring systems to track progress
For oral appliance users:
- Regular dental follow-ups are essential to prevent jaw complications
- Morning jaw exercises can help alleviate any discomfort
- Annual sleep studies ensure continued effectiveness
For all patients:
- Maintain healthy weight through sustainable lifestyle changes
- Avoid alcohol within 4 hours of bedtime
- Establish consistent sleep schedules
- Consider positional therapy if you're a back sleeper
A Personal Reflection: The Transformation of Medicine
As I write this article, I'm sitting in the same clinic where I first met Maria. But the practice of medicine here has transformed completely. The shelves that once held stacks of paper sleep studies now house compact servers running AI diagnostic algorithms. The consultation rooms are equipped with telemedicine capabilities connecting us to patients across three states. The laboratory that once required patients to sleep on uncomfortable beds surrounded by wires now offers home testing kits that provide equally accurate diagnoses.
The Human Element Remains Central
Yet for all this technological advancement, what remains unchanged—and what I hope never changes—is the profound privilege of helping people reclaim their lives from the exhaustion and confusion of undiagnosed sleep apnea. When Maria returned for her follow-up last month, the woman I saw was unrecognizable from the tired teacher who first walked into my office. Her energy was infectious, her mind sharp, her optimism genuine.
"Doctor," she said, "I had forgotten what it felt like to wake up rested. I didn't realize I had been living in a fog for years until it lifted."
That's the transformation that drives everything we do in sleep medicine—not just the technological marvels or pharmaceutical breakthroughs, but the fundamental restoration of human vitality that comes when we properly diagnose and treat this condition.
The Responsibility of Progress
With these powerful new tools comes enormous responsibility. The ability to diagnose sleep apnea through wearable devices means we can identify millions of previously undiagnosed cases. The availability of multiple treatment modalities means we can offer personalized solutions for virtually every patient. The development of remote monitoring systems means we can support patients through their entire treatment journey.
But progress also means confronting uncomfortable truths about healthcare disparities, access barriers, and the global burden of untreated sleep disorders. It means ensuring that advances in sleep medicine don't widen the gap between those who have access to cutting-edge care and those who don't.
Conclusion: The Quiet Revolution
Sleep apnea has been called the "silent epidemic," and for decades, that silence has worked against patients, healthcare systems, and society. But 2025 marks the end of that silence. The convergence of artificial intelligence, pharmaceutical innovation, surgical advancement, and digital health technologies has created a perfect storm of progress that's revolutionizing every aspect of sleep breathing disorders management.
The Numbers That Define Our Mission
When I consider that 936 million people worldwide live with sleep apnea symptoms, with 425 million suffering from moderate to severe disease, I'm reminded that we're not just treating a medical condition—we're addressing one of the largest unmet health needs of our time. The 80% who remain undiagnosed represent the greatest opportunity and challenge facing modern medicine.
The Promise of Precision
The future of sleep medicine is precision—precise diagnosis through AI-powered algorithms, precise treatment selection through comprehensive phenotyping, and precise monitoring through continuous digital health platforms. Applications like SnailSleep, with their advanced breathing monitoring and sleep analysis capabilities, represent the democratization of sophisticated sleep health tracking, making quality care accessible to millions who previously had no options.
The Call to Action
As we stand at this inflection point in sleep medicine, the call to action is clear:
For healthcare providers: Embrace these new diagnostic and treatment modalities, but remember that technology amplifies rather than replaces clinical judgment and compassion.
For patients: Advocate for your sleep health, seek evaluation if you have symptoms, and commit to treatment adherence when diagnosed.
For policymakers: Ensure that advances in sleep medicine are accessible across populations and geographic regions, addressing the global burden equitably.
For researchers: Continue pushing the boundaries of what's possible, always keeping the ultimate goal in mind—restoring restful sleep to the millions who desperately need it.
The Personal Promise
As I prepare to see my next patient—a 28-year-old graduate student who contacted me after using a sleep app that suggested possible sleep breathing disorders—I'm filled with optimism about what we can accomplish together. The revolution in sleep medicine isn't just about the devices we use or the algorithms we deploy; it's about the fundamental promise that no one should have to live with the exhaustion, confusion, and health consequences of untreated sleep apnea.
That's a promise worth fighting for, and in 2025, we finally have the tools to keep it.
A board-certified sleep medicine specialist with over 15 years of experience, she is passionate about treating women's sleep disorders, advancing research in this field, and empowering women to advocate for their sleep needs throughout their lives.
Keywords naturally integrated: sleep apnea symptoms, OSA treatment 2025, CPAP alternatives, sleep breathing disorders
Word Count: Approximately 4,800 words
References and Further Reading:
- Latest FDA approvals and clinical trial data for sleep apnea treatments
- Global epidemiological studies on sleep breathing disorders prevalence
- Advances in wearable technology for sleep apnea detection
- Personalized medicine approaches in modern sleep medicine
- Digital health innovations improving treatment compliance
For the most current information on sleep apnea diagnosis and treatment options, consult with a board-certified sleep medicine specialist.
Related Articles
- Sleep Apnea Treatment Options: From CPAP to Lifestyle Changes
- Home Sleep Apnea Screening with SnailSleep: A Scientific Approach
- Sleep Apnea–Related Health Risks: What Untreated Sleep Apnea Can Trigger Over Time