Sleep and Immunity: Enhanced T-Cell Activation During Sleep
Published by Dr. Robert Kim | Immunology and Sleep Research Specialist
 T-cell activation during sleep
T-cell activation during sleep
The relationship between sleep and immune function is one of the most fascinating areas of modern sleep science. Research has increasingly shown that sleep is not just a passive state of rest, but an active period during which critical immune processes occur. This comprehensive guide explores how sleep enhances T-cell activation, strengthens our immune defenses, and plays a crucial role in maintaining overall health and resistance to disease.
The Immune System: Our Body's Defense Network
The immune system is a complex network of cells, tissues, and organs that work together to protect the body from harmful invaders such as bacteria, viruses, fungi, and parasites. It consists of two main branches:
Innate Immunity
- First line of defense: Physical barriers (skin, mucous membranes)
- Rapid response: Non-specific protection against a wide range of pathogens
- Inflammatory response: Immediate reaction to tissue damage or infection
Adaptive Immunity
- Specific response: Targets specific pathogens
- Memory formation: Remembers previous encounters with pathogens
- T-cells and B-cells: Key players in adaptive immune responses
 Immune system sleep benefits
Immune system sleep benefits
T-Cells: The Commanders of Adaptive Immunity
T-cells, or T lymphocytes, are white blood cells that play a central role in the adaptive immune response. They are produced in the bone marrow and mature in the thymus gland, hence the name "T-cell."
Types of T-Cells
Helper T-Cells (CD4+):
- Coordinate immune responses
- Help activate other immune cells
- Produce cytokines that regulate immune activity
- Essential for antibody production by B-cells
Cytotoxic T-Cells (CD8+):
- Directly kill infected cells
- Target cells displaying foreign antigens
- Play crucial role in viral infections and cancer surveillance
Regulatory T-Cells (Tregs):
- Suppress excessive immune responses
- Prevent autoimmune reactions
- Maintain immune tolerance
Memory T-Cells:
- Remember previous infections
- Provide rapid response upon re-exposure
- Long-lived cells that persist for years
Sleep and T-Cell Function: The Scientific Evidence
Circadian Regulation of T-Cell Activity
Research has shown that T-cell function follows a circadian rhythm, with peak activity occurring during sleep:
Nighttime T-Cell Activation:
- T-cell proliferation increases during sleep
- Enhanced production of cytokines and chemokines
- Improved antigen recognition and response
- Better memory T-cell formation
Daytime T-Cell Suppression:
- Reduced T-cell activity during wakefulness
- Lower cytokine production
- Decreased proliferation rates
- Focus on other physiological processes
 Sleep loss immune impact
Sleep loss immune impact
Sleep Stages and Immune Function
Different stages of sleep appear to have distinct effects on immune function:
Deep Sleep (N3):
- Peak T-cell activation
- Enhanced cytokine production
- Optimal immune memory formation
- Tissue repair and regeneration
REM Sleep:
- Continued immune activity
- Emotional memory processing
- Integration of immune responses
- Stress hormone regulation
Light Sleep (N1, N2):
- Transition periods
- Moderate immune activity
- Preparation for deeper sleep stages
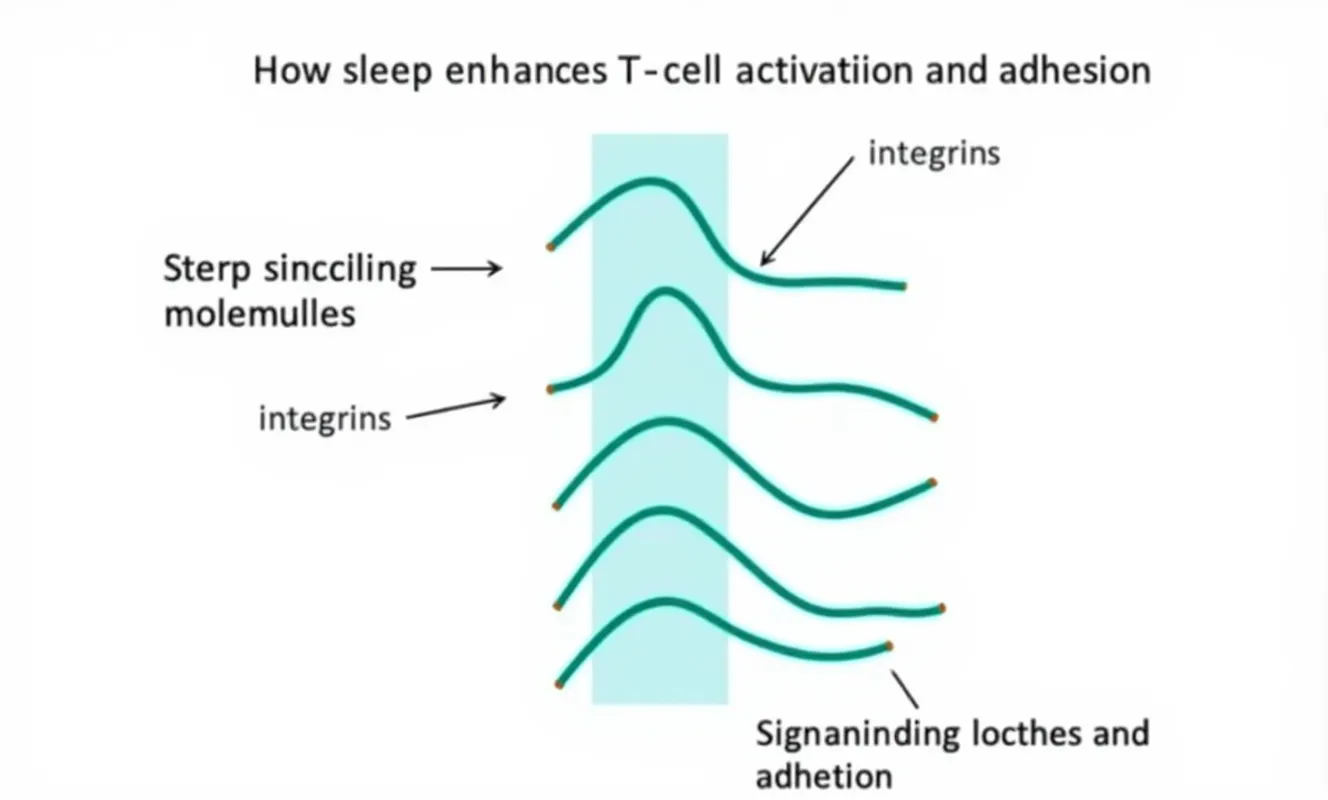
Mechanisms of Sleep-Enhanced T-Cell Activation
Hormonal Regulation
Melatonin:
- Production: Secreted by pineal gland during darkness
- Immune effects: Enhances T-cell proliferation and cytokine production
- Antioxidant properties: Protects immune cells from oxidative damage
- Timing: Peak levels during sleep coincide with peak T-cell activity
Growth Hormone:
- Secretion: Primarily occurs during deep sleep
- T-cell effects: Promotes T-cell development and function
- Tissue repair: Essential for immune system maintenance
- Metabolic regulation: Influences immune cell energy metabolism
Cortisol:
- Diurnal pattern: Lowest levels during sleep
- Immune regulation: Reduces inflammation during sleep
- T-cell modulation: Influences T-cell differentiation and function
- Stress response: Links sleep quality to immune resilience
Neurotransmitter Effects
GABA (Gamma-Aminobutyric Acid):
- Primary inhibitory neurotransmitter: Promotes sleep and relaxation
- Immune effects: May enhance T-cell function during sleep
- Stress reduction: Lower stress levels improve immune function
- Sleep quality: Better sleep leads to enhanced immune responses
Serotonin:
- Mood regulation: Influences stress and anxiety levels
- Immune modulation: Affects T-cell cytokine production
- Sleep-wake cycles: Regulates circadian rhythms
- Gut-brain axis: Links digestive health to immune function
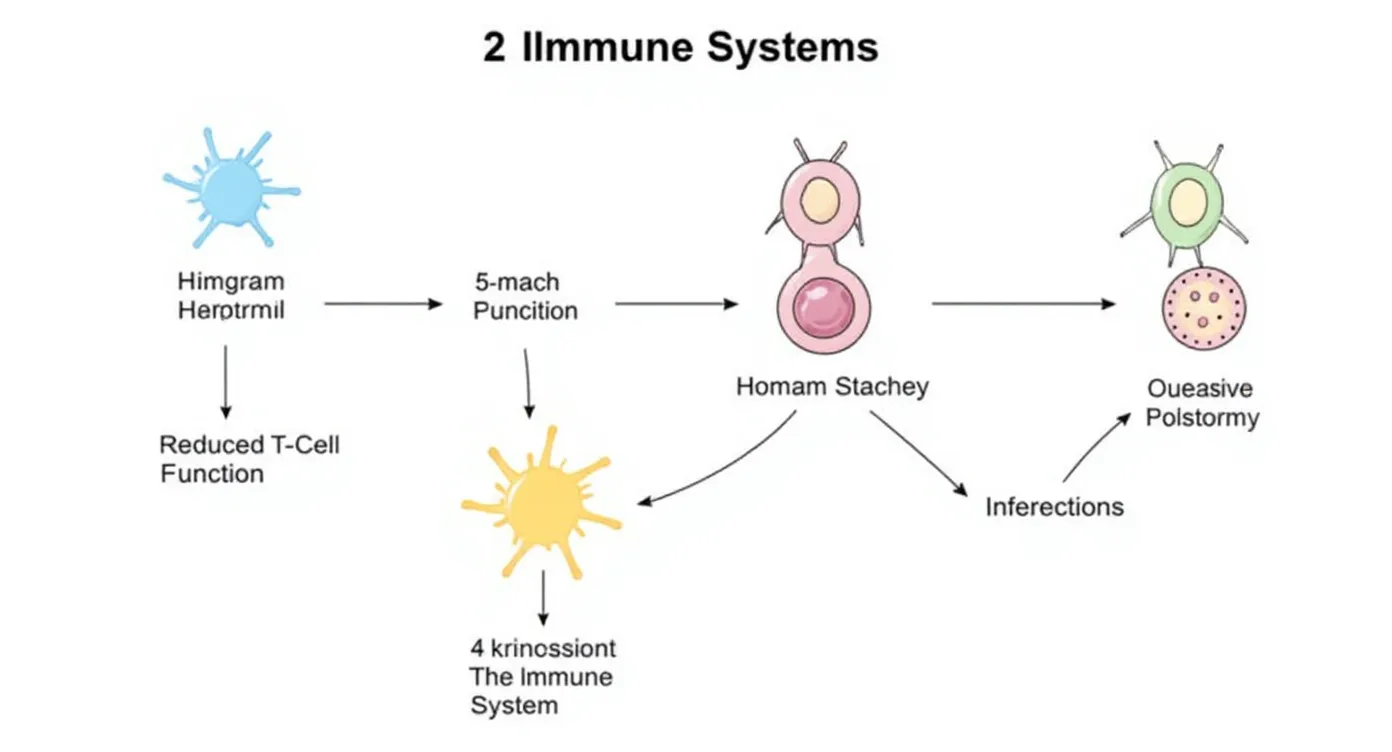
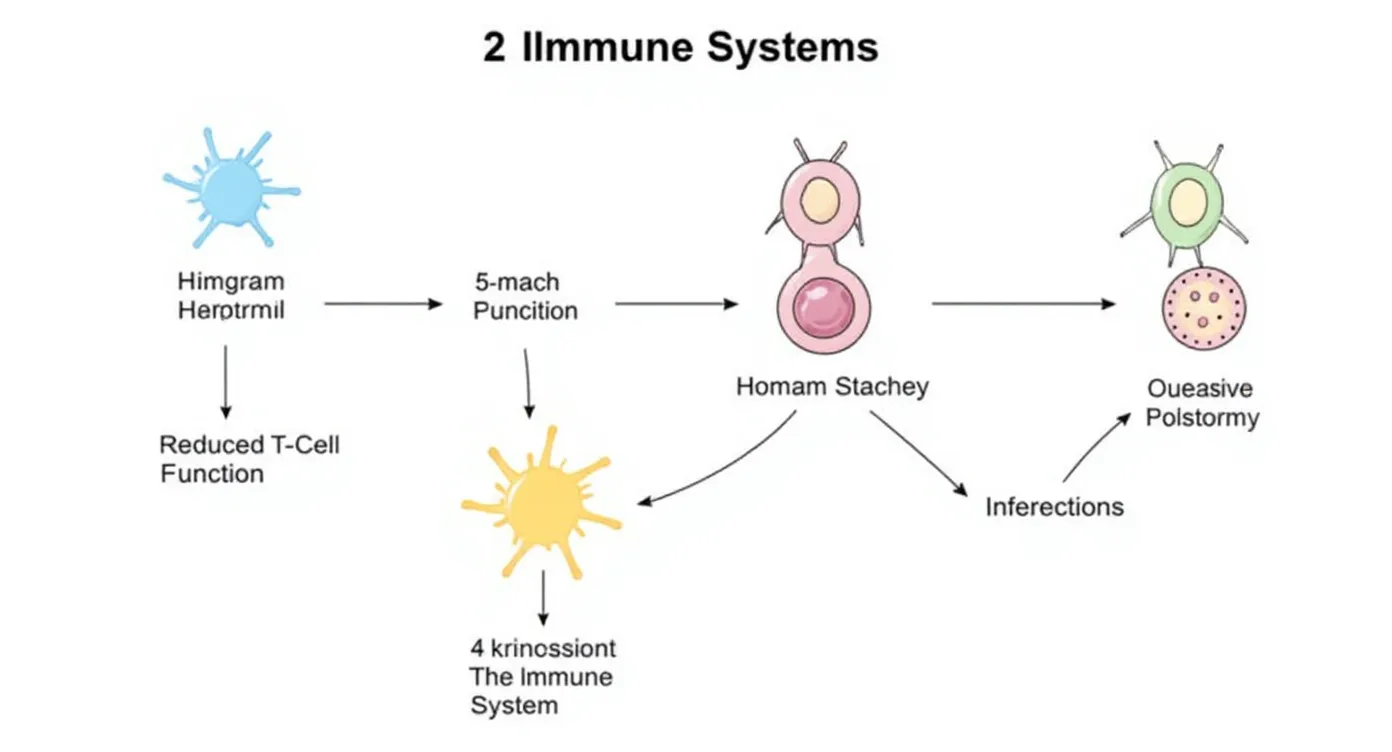
Sleep Deprivation and Immune Suppression
Acute Sleep Deprivation (1-2 nights)
T-Cell Function Impairment:
- Reduced T-cell proliferation
- Decreased cytokine production
- Impaired antigen recognition
- Lower memory T-cell formation
Inflammatory Response:
- Increased pro-inflammatory cytokines
- Elevated C-reactive protein levels
- Enhanced inflammatory markers
- Potential tissue damage
 Sleep loss immune impact
Sleep loss immune impact
Chronic Sleep Deprivation (weeks to months)
Long-term Immune Consequences:
- Persistent T-cell dysfunction
- Chronic inflammation
- Increased infection risk
- Reduced vaccine effectiveness
- Higher cancer risk
Metabolic Effects:
- Insulin resistance
- Weight gain
- Increased stress hormones
- Compromised immune cell energy metabolism
Practical Implications for Health
Infection Resistance
Viral Infections:
- Adequate sleep enhances T-cell response to viruses
- Better memory T-cell formation for future protection
- Improved cytokine production for viral clearance
- Enhanced natural killer cell activity
Bacterial Infections:
- Stronger T-cell-mediated immune responses
- Better coordination between innate and adaptive immunity
- Enhanced antibody production through T-cell help
- Improved tissue repair and recovery
Vaccine Effectiveness
Enhanced Response:
- Better T-cell activation after vaccination
- Improved memory T-cell formation
- Stronger and longer-lasting immunity
- More effective protection against disease
Timing Considerations:
- Sleep quality before vaccination matters
- Consistent sleep schedule improves response
- Adequate sleep after vaccination enhances memory formation
Autoimmune Disease
Immune Regulation:
- Sleep helps maintain immune tolerance
- Regulatory T-cell function is enhanced during sleep
- Reduced inflammation prevents autoimmune reactions
- Better stress management through sleep
Optimizing Sleep for Immune Health
Sleep Duration Recommendations
Adults (18-64 years): 7-9 hours per night Older adults (65+): 7-8 hours per night Teenagers (14-17 years): 8-10 hours per night School-age children (6-13 years): 9-11 hours per night
Sleep Quality Factors
Environment:
- Cool, dark, and quiet bedroom
- Comfortable mattress and pillows
- Optimal temperature (60-67°F/15-19°C)
- Minimal light exposure
Timing:
- Consistent sleep schedule
- Regular bedtime routine
- Avoid large meals and caffeine before bed
- Regular exercise (but not close to bedtime)
Behavior:
- Use bed only for sleep and intimacy
- Avoid electronic devices before bedtime
- Practice relaxation techniques
- Manage stress and anxiety
Circadian Rhythm Optimization
Light Exposure:
- Bright light exposure in the morning
- Reduce blue light exposure in the evening
- Maintain regular exposure to natural light
- Use blackout curtains for complete darkness
Social Rhythms:
- Consistent meal times
- Regular exercise schedule
- Stable social activities
- Avoid major schedule disruptions
Special Considerations
Shift Work and Immune Function
Challenges:
- Disrupted circadian rhythms
- Inconsistent sleep patterns
- Increased stress and fatigue
- Higher infection rates
Mitigation Strategies:
- Maintain consistent sleep schedule when possible
- Use light therapy to regulate circadian rhythms
- Optimize sleep environment during day sleep
- Regular health monitoring
Travel and Jet Lag
Effects on Immunity:
- Disrupted sleep-wake cycles
- Reduced T-cell function
- Increased infection risk
- Delayed recovery from illness
Prevention:
- Gradual adjustment to new time zones
- Light exposure management
- Melatonin supplementation (consult healthcare provider)
- Maintain healthy sleep habits
Age-Related Changes
Older Adults:
- Reduced deep sleep
- Altered immune function
- Higher infection risk
- Slower recovery from illness
Optimization Strategies:
- Focus on sleep quality over quantity
- Regular exercise and physical activity
- Healthy diet and nutrition
- Stress management and social engagement
Research Frontiers
Emerging Areas of Study
Sleep and Cancer Immunity:
- T-cell surveillance during sleep
- Sleep's role in cancer prevention
- Treatment response and sleep quality
- Circadian timing of cancer therapies
Sleep and Autoimmune Disease:
- Sleep quality in autoimmune conditions
- Sleep interventions for disease management
- Circadian disruption and disease flares
- Personalized sleep recommendations
Sleep and Mental Health:
- Bidirectional relationship with immune function
- Sleep interventions for mood disorders
- Stress-immune-sleep interactions
- Therapeutic sleep optimization
Conclusion
The relationship between sleep and immune function represents one of the most important discoveries in modern sleep science. Sleep is not merely a time of rest, but an active period during which critical immune processes occur, particularly the activation and enhancement of T-cell function.
Understanding this relationship has profound implications for health and disease prevention. By optimizing our sleep habits, we can enhance our immune defenses, improve our resistance to infections, and support our body's natural healing processes.
The evidence is clear: adequate, high-quality sleep is essential for optimal immune function. Whether you're looking to prevent illness, enhance vaccine effectiveness, or simply maintain good health, prioritizing sleep should be at the top of your wellness strategy.
Key Takeaways
- Sleep is essential for optimal T-cell function and immune health
- T-cell activation peaks during sleep, particularly deep sleep
- Sleep deprivation significantly impairs immune function
- Adequate sleep enhances vaccine effectiveness and infection resistance
- Sleep quality is as important as sleep quantity for immune health
- Circadian rhythms play a crucial role in immune function
- Optimizing sleep can help prevent illness and improve recovery
- Sleep interventions may be valuable for immune-related conditions
References
- Besedovsky, L., et al. (2012). Sleep and immune function. Pflügers Archiv - European Journal of Physiology, 463(1), 121-137.
- Irwin, M. R. (2019). Sleep and inflammation: partners in sickness and in health. Nature Reviews Immunology, 19(11), 702-715.
- Besedovsky, L., et al. (2019). The sleep-immune crosstalk in health and disease. Physiological Reviews, 99(3), 1325-1380.
- Dimitrov, S., et al. (2019). Gαs-coupled receptor signaling and sleep regulate integrin activation of human antigen-specific T cells. Journal of Experimental Medicine, 216(3), 517-526.
- National Sleep Foundation. (2020). Sleep in America Poll: Sleep and Immune Function.
Related Articles
- Sleep and Immune System: How Sleep Helps Fight Disease
- The Complete Guide to Circadian Rhythm Optimization for Better Sleep
- Diet and Sleep: Foods That Help You Sleep Better
