The Hidden Dangers of Snoring: A Comprehensive Guide to Sleep-Disordered Breathing
I'll never forget the phone call I received from Sarah three months ago. Her husband Mark had been a heavy snorer for years—the kind that rattled windows and sent her to the guest bedroom most nights. "It's just snoring," they'd always said. "Men snore. It's normal."
Then Mark had a heart attack at 44.
As his cardiologist reviewed his case, the dots connected in a way that startled everyone. Mark's "harmless" snoring had been systematically damaging his cardiovascular system for over a decade. His blood pressure, which seemed controllable with medication, was actually being driven by something no one had considered: his airways were collapsing dozens of times each night.
Mark's story isn't unique. Across the globe, 57% of men and 40% of women snore regularly. That's over 7 billion people worldwide. But here's what most don't realize: snoring isn't just about noise. It's often a warning sign of something far more serious happening inside your body.
What Your Body Is Really Telling You
When most people think about snoring, they picture an annoying nighttime sound that disrupts sleep. The reality is considerably more complex—and concerning.
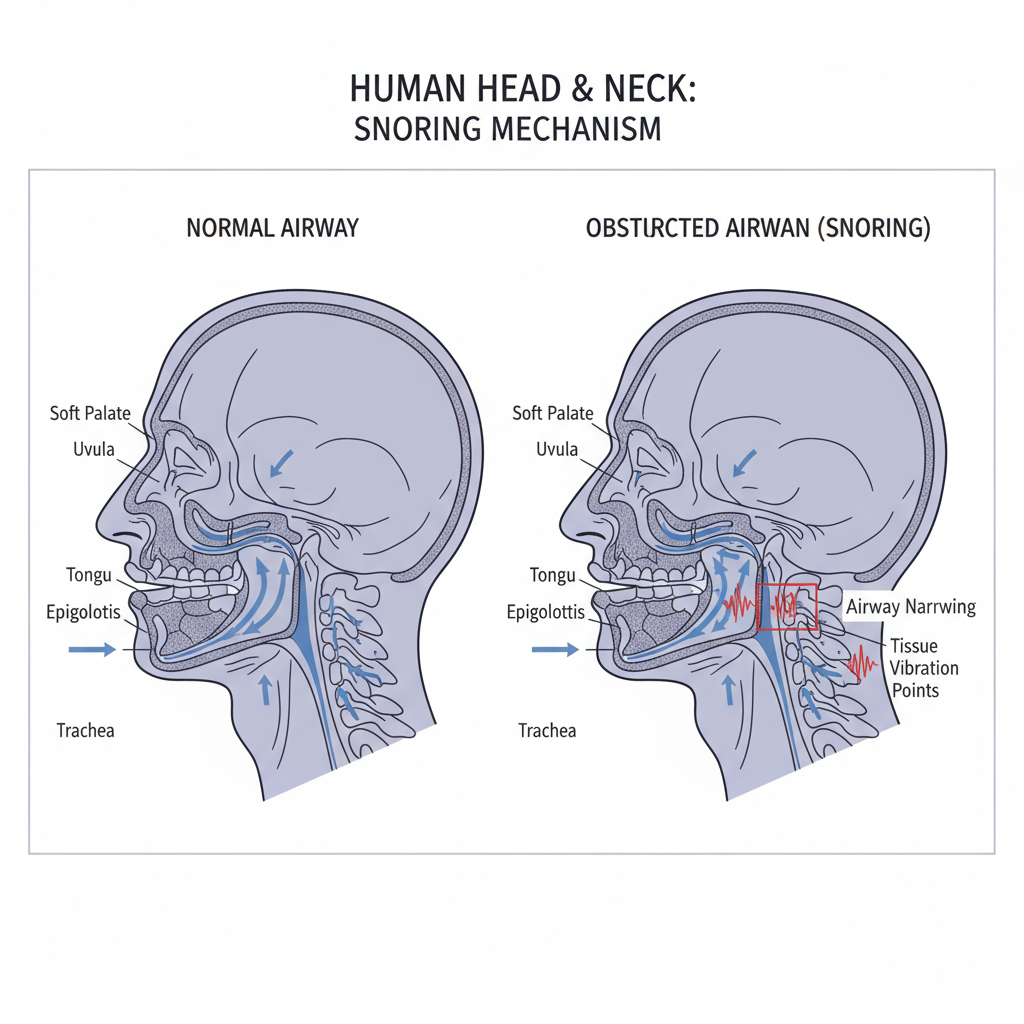
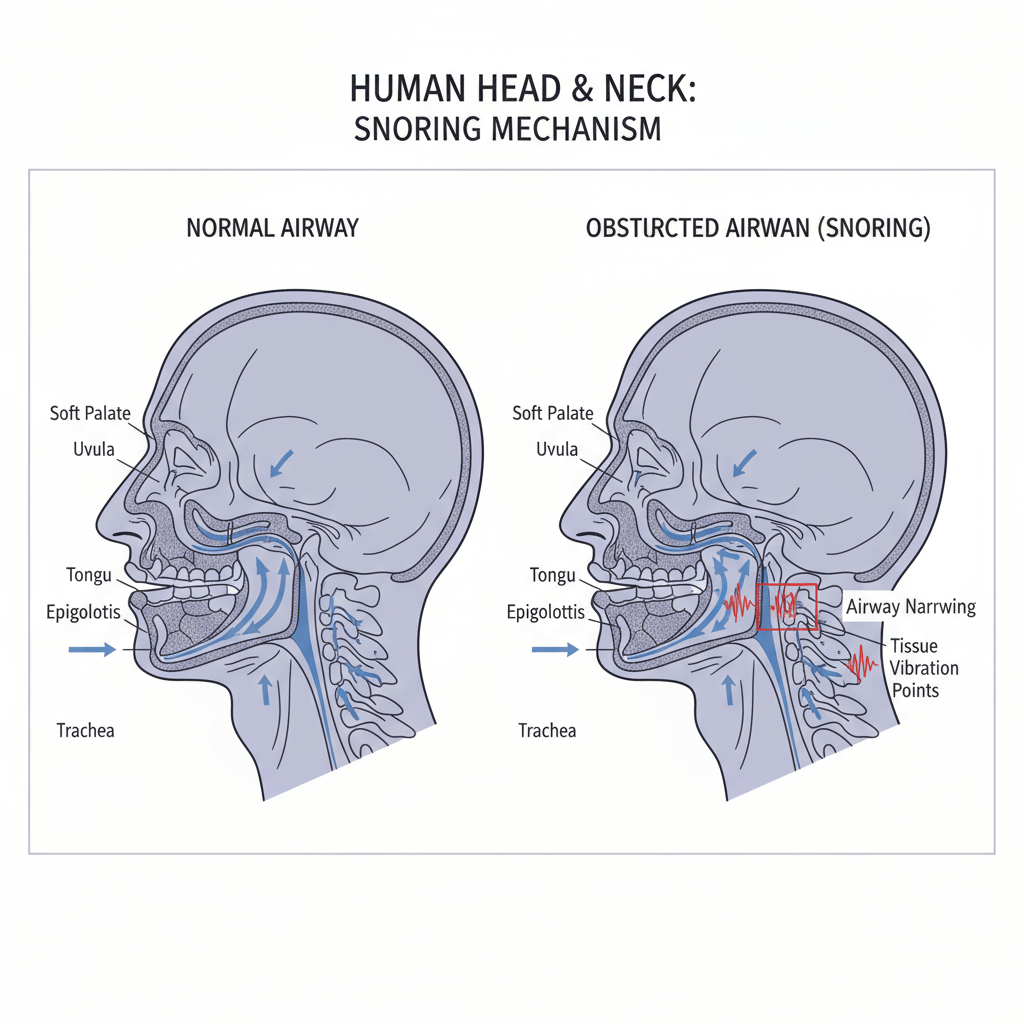 Snoring Anatomy Professional Diagram
Snoring Anatomy Professional Diagram
The Mechanics of Mayhem
Snoring occurs when air can't move freely through your nose and throat during sleep. As the muscles in your mouth, tongue, and throat relax, they can partially block your airway. When you breathe, these relaxed tissues vibrate, creating that characteristic sound we all recognize.
But here's where it gets serious. That vibration? It's not just creating noise—it's creating trauma. Recent research published in Nature Digital Medicine shows that the mechanical vibrations from snoring can actually damage blood vessel walls, particularly in the carotid arteries that supply blood to your brain.
The Cardiovascular Time Bomb
A groundbreaking 2024 study involving 12,287 participants used objective sleep monitoring technology to reveal something that should alarm everyone: regular snoring increases the risk of uncontrolled hypertension by 87%. This association exists completely independent of sleep apnea.
Let me put that in perspective. Even if you don't stop breathing during sleep—even if you just snore consistently—you're nearly doubling your risk of dangerous blood pressure levels. The study found that people with high snoring frequency showed blood pressure increases of 3.8 mmHg systolic and 4.5 mmHg diastolic compared to quiet sleepers.
Those numbers might seem small, but in cardiovascular medicine, they're massive. A 3.8 mmHg increase in systolic blood pressure translates to approximately 15% increased stroke risk and 10% increased heart attack risk at the population level.
The Global Health Crisis Hidden in Plain Sight
Here's something that should fundamentally change how we think about snoring: 70% of regular snorers are eventually diagnosed with sleep apnea. This isn't correlation—it's progression. Snoring often represents the early stage of a condition that affects an estimated 1 billion adults worldwide.
Sleep apnea occurs when your airway doesn't just vibrate—it completely collapses, cutting off oxygen to your brain and vital organs. Your body responds with a surge of stress hormones, your blood pressure spikes, and your heart rate increases dramatically. This happens not once or twice, but potentially hundreds of times per night.
The most troubling aspect? 80-90% of people with moderate to severe sleep apnea remain undiagnosed. They're walking around with a condition that triples their risk of stroke, doubles their risk of heart failure, and increases their overall mortality risk by 54%.
The Ripple Effects: Beyond the Snorer
What struck me most about working with couples dealing with snoring isn't just the health impacts on the snorer—it's the collateral damage to their partners and families.
The Partner's Plight
Research shows that 70% of snorers' partners experience sleep quality deterioration. But it goes deeper than just interrupted sleep. Partners of habitual snorers show:
- 3 times higher rates of insomnia symptoms compared to the general population
- Increased daytime fatigue and cognitive impairment
- Higher stress hormone levels (cortisol) upon morning awakening
- More frequent use of sleep medications
- Higher rates of relationship dissatisfaction
One study tracked couples where one partner snored heavily. After six months, the non-snoring partner showed measurable changes in immune function and increased inflammation markers—their health was literally being affected by their partner's sleep disorder.
The Family Dynamic
Children in households with a snoring parent show increased rates of:
- Sleep anxiety and bedtime resistance
- Behavioral problems during the day
- Academic performance issues
- Their own sleep disorders later in life
It's a cycle that perpetuates across generations, with sleep disorders often running in families not just due to genetics, but due to normalized poor sleep habits.
Breaking Down the Science: Types and Triggers
Not all snoring is created equal. Modern sleep medicine recognizes distinct patterns that carry different health implications.
Primary (Isolated) Snoring
This occurs without accompanying breathing interruptions. While less dangerous than sleep apnea, recent research shows it's not benign. The cardiovascular risks I mentioned earlier—the 87% increased hypertension risk—apply to this category.
Sleep Apnea-Associated Snoring
This is snoring that occurs with, or signals, complete airway obstruction. It's characterized by:
- Loud, irregular snoring patterns
- Periods of silence followed by gasping or choking sounds
- Multiple awakenings during the night
- Excessive daytime sleepiness despite adequate time in bed
Gender and Age Patterns
The research reveals fascinating patterns in how snoring affects different demographics:
Men vs. Women:
- Young women (under 40) with mild sleep apnea show significantly more snoring during deep sleep (N3 stage) than men
- Post-menopausal women experience a sharp increase in snoring frequency
- Men show higher rates of upper airway collapse and more sensitive central chemoreceptors
Age Progression: Sleep apnea prevalence increases dramatically with age:
- Ages 20-44: 3.2% of men, 0.6% of women
- Ages 45-64: 11.3% of men, 2.0% of women
- Ages 65-100: 18.1% of men, 7.0% of women
Anatomical and Environmental Triggers
Several factors contribute to snoring development:
Structural Issues:
- Deviated nasal septum
- Enlarged tonsils or adenoids
- Low soft palate or enlarged uvula
- Receding chin or small jaw structure
Lifestyle Factors:
- Obesity (even moderate weight gain can trigger snoring)
- Alcohol consumption (relaxes throat muscles)
- Sleeping medications
- Chronic nasal congestion
- Sleep position (back sleeping worsens most snoring)
The Treatment Revolution: From CPAP to Cutting-Edge Solutions
The landscape of snoring and sleep apnea treatment has transformed dramatically in recent years. Gone are the days when CPAP (Continuous Positive Airway Pressure) was the only viable option for serious cases.
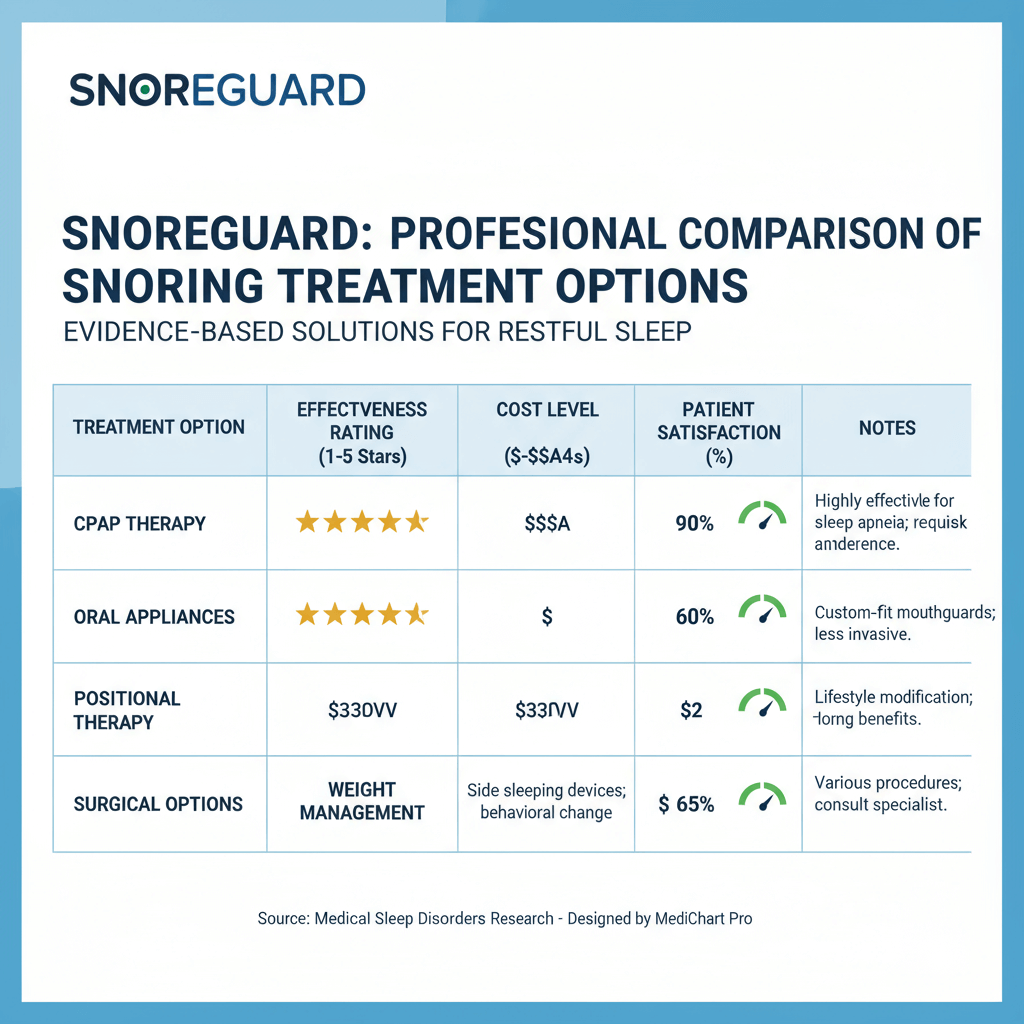 Snoring Treatment Comparison Chart
Snoring Treatment Comparison Chart
The CPAP Gold Standard
CPAP therapy remains the most effective treatment for moderate to severe sleep apnea, with success rates above 90% when properly used. The machine delivers pressurized air through a mask, keeping airways open throughout the night.
However, compliance remains challenging. Studies show that 30-50% of CPAP users struggle with long-term adherence due to:
- Mask discomfort and air leaks
- Feeling claustrophobic
- Difficulty traveling with equipment
- Skin irritation and dry mouth
- Partner complaints about noise
Breakthrough Pharmaceutical Options
December 2024 marked a historic moment in sleep medicine: the FDA approved Zepbound (tirzepatide) as the first medication specifically for treating obesity-related sleep apnea in adults.
The SURMOUNT-OSA clinical trial, published in the New England Journal of Medicine, showed remarkable results:
- 25.3 events per hour reduction in Apnea-Hypopnea Index (AHI) compared to 5.3 with placebo
- Treatment difference of -20.0 events/hour (95% CI: -25.8 to -14.2)
- Significant improvements in sleep quality and daytime alertness
The drug works by activating GLP-1 and GIP hormone receptors, reducing appetite and food intake. By addressing the obesity component of sleep apnea, it tackles one of the root causes rather than just managing symptoms.
Innovative Device Solutions
Oral Appliance Therapy: Custom-fitted dental devices that advance the lower jaw and tongue, keeping the airway open. Success rates range from 60-80% for mild to moderate cases, with much higher patient satisfaction than CPAP.
Hypoglossal Nerve Stimulation: A surgically implanted device that stimulates the nerve controlling tongue movement, preventing airway collapse. Reserved for CPAP-intolerant patients with specific anatomical criteria:
- AHI between 15-65 events per hour
- BMI less than 32 kg/m²
- Specific upper airway anatomy requirements
Success rates approach 70-80% for appropriate candidates, with high patient satisfaction scores.
Positional Therapy Advances
New research shows that 30-40% of sleep apnea cases are position-dependent, occurring primarily when sleeping on the back. Modern positional therapy devices use gentle vibration to encourage side sleeping without fully waking the user.
DIY Solutions That Actually Work (And Those That Don't)
Let's address the elephant in the room: internet "cures" for snoring. The wellness industry is flooded with products making bold claims. Here's what the evidence actually supports:
Proven Interventions
Weight Management: Even modest weight loss can have dramatic effects. A 10% reduction in body weight typically reduces AHI by 26%. For many people, losing 15-20 pounds can eliminate mild to moderate sleep apnea entirely.
Sleep Position Training: Sleeping on your side reduces snoring frequency by 50-70% in position-dependent cases. Simple solutions like sewing a tennis ball into the back of your pajama shirt remain surprisingly effective.
Nasal Dilators and Strips: External nasal strips can reduce snoring by improving nasal airflow, particularly helpful for people with chronic congestion or structural nasal issues. Internal nasal dilators show even better results in some studies.
Throat Exercises (Myofunctional Therapy): Specific exercises targeting mouth, tongue, and throat muscles can reduce snoring frequency by 40-50% and AHI by 20-30% in mild cases. These include:
- Tongue position training
- Soft palate strengthening
- Breathing pattern modification
Popular Myths That Don't Work
Anti-Snoring Pillows: While proper pillow height can help with positioning, specialized "anti-snoring" pillows show no evidence of effectiveness beyond regular supportive pillows.
Throat Sprays and Lubricants: Despite aggressive marketing, no clinical evidence supports their effectiveness for consistent snoring reduction.
Magnetic Nose Clips: No scientific basis for effectiveness. Save your money.
Essential Oils: While some oils may help with nasal congestion, they don't address the fundamental mechanical issues causing snoring.
When Professional Help Becomes Critical
Here's my professional advice on when snoring transitions from nuisance to medical emergency:
Red Flag Symptoms
Immediate Medical Attention Required:
- Gasping or choking sounds during sleep
- Witnessed breathing pauses longer than 10 seconds
- Severe daytime sleepiness (falling asleep while driving, talking, eating)
- Morning headaches combined with loud snoring
- High blood pressure that's difficult to control with medication
Schedule Professional Evaluation:
- Partner reports loud, irregular snoring patterns
- Unrefreshing sleep despite 7-8 hours in bed
- Difficulty concentrating or memory problems
- Weight gain combined with increased snoring
- Snoring that developed suddenly or worsened significantly
The Diagnostic Process
Modern sleep medicine offers several diagnostic approaches:
Home Sleep Apnea Testing (HSAT): Convenient, cost-effective screening for sleep apnea using portable monitors. Appropriate for straightforward cases without complicating factors.
Laboratory Polysomnography (PSG): The gold standard for complex cases, providing detailed information about sleep architecture, breathing patterns, heart rhythm, and movement disorders.
Drug-Induced Sleep Endoscopy (DISE): A procedure where the upper airway is examined while you're in a medication-induced sleep state, allowing precise identification of collapse locations.
The Technology Revolution: Professional vs. Consumer Monitoring
The past five years have seen explosive growth in consumer sleep tracking technology. But how do these devices compare to professional-grade monitoring?
Consumer Device Capabilities
Recent analysis of 62 wearable devices showed:
- 87.2% accuracy for sleep/wake detection across leading devices
- Oura Ring leads with 76-79.5% consistency in sleep stage detection
- Apple Watch and Samsung Galaxy Watch now FDA-approved for sleep apnea screening
These approvals represent a paradigm shift. For the first time, you can receive medically-validated screening for sleep disorders from your wrist.
Professional Platform Advantages
This is where comprehensive sleep platforms like SnailSleep excel. With over 80 million global users, SnailSleep has access to sleep data patterns impossible to achieve in traditional clinical settings.
Advanced professional monitoring provides:
- Breathing pattern analysis beyond simple apnea detection
- Heart rate variability tracking during different sleep stages
- Environmental factor correlation (temperature, humidity, sound)
- Long-term trend analysis showing gradual changes over months or years
- Personalized intervention recommendations based on individual sleep architecture
The key difference isn't just accuracy—it's actionability. While consumer devices might tell you that you snored, professional platforms can identify specific triggers, optimal treatment timing, and personalized intervention strategies.
The Economics of Untreated Snoring
The financial implications of ignoring snoring and sleep apnea are staggering:
Individual Healthcare Costs:
- Sleep apnea patients average $2,720 more in annual healthcare expenses
- Undiagnosed patients show 50% higher medical utilization rates
- CPAP treatment typically pays for itself within 2-3 years through reduced medical costs
Societal Impact:
- $869 billion annually in productivity losses from untreated sleep apnea
- $159 billion in traffic accident costs (1,400 deaths annually)
- $34 billion in CPAP treatment costs (projected to reach $111 billion by 2030)
Insurance Considerations: Most insurance plans now cover sleep apnea diagnosis and treatment, recognizing the long-term cost savings. Many also cover newer treatments like oral appliances and hypoglossal nerve stimulation for appropriate candidates.
Your Personal Action Plan
Based on current evidence and clinical experience, here's my systematic approach to addressing snoring concerns:
Step 1: Assessment (Week 1-2)
- Document the problem: Record snoring frequency, intensity, and patterns
- Partner observations: Note any breathing pauses, gasping, or position dependency
- Daytime symptoms: Track energy levels, concentration, and mood
- Consider professional monitoring: Use objective measurement tools for baseline data
Step 2: Conservative Interventions (Weeks 3-8)
- Optimize sleep position: Train yourself to sleep on your side
- Address nasal congestion: Use saline rinses, consider nasal strips
- Weight management: If overweight, aim for 1-2 pounds per week loss
- Sleep hygiene: Consistent bedtime, optimal sleep environment
- Alcohol reduction: Limit alcohol within 3 hours of bedtime
Step 3: Professional Evaluation (If needed after 4-6 weeks)
- Primary care consultation: Discuss symptoms and get referral if needed
- Sleep study: Home testing for straightforward cases, lab study for complex situations
- ENT evaluation: If structural abnormalities are suspected
- Dental consultation: For oral appliance candidacy assessment
Step 4: Treatment Implementation
- Follow through: Whatever treatment is recommended, give it adequate time to work
- Monitor progress: Track improvements in sleep quality and daytime symptoms
- Adjust as needed: Work with your healthcare team to optimize treatment
- Long-term maintenance: Most successful treatments require ongoing adherence
The Future of Snoring Treatment
We're entering an exciting era of personalized sleep medicine. Genetic testing can now identify individuals at higher risk for sleep apnea. Artificial intelligence analyzes sleep patterns to predict treatment success. Advanced imaging techniques help surgeons plan procedures with unprecedented precision.
Emerging Therapies:
- Combination drug therapy: Multiple medications targeting different apnea mechanisms
- Neurostimulation advances: More refined control of upper airway muscles
- Biomarker-guided treatment: Using blood tests to optimize therapy selection
- Precision surgery: AI-guided procedures targeting individual anatomical issues
Technology Integration:
- Smart home integration: Environmental controls responding to real-time sleep data
- Predictive analytics: Warning systems for apnea episodes before they occur
- Telemedicine monitoring: Remote adjustment of treatments based on objective data
The Bottom Line: Your Health Is Worth More Than a Good Night's Sleep
If you take away one thing from this comprehensive guide, let it be this: snoring is not normal, and it's not harmless.
Yes, some people snore occasionally without serious consequences. But consistent, loud snoring—especially when combined with other symptoms—represents your body's distress signal that something isn't right with one of your most fundamental biological processes: breathing during sleep.
The research is overwhelming: untreated sleep-disordered breathing contributes to heart disease, stroke, diabetes, depression, and premature death. The good news? We have more effective treatment options than ever before, ranging from simple lifestyle modifications to breakthrough pharmaceutical interventions.
The question isn't whether you can live with snoring—it's whether you want to risk the consequences of leaving it untreated. In most cases, addressing snoring and sleep apnea doesn't just improve sleep quality; it can literally add years to your life while dramatically improving the quality of those years.
Your partner will sleep better, your cardiovascular system will thank you, and you'll wake up feeling like the person you remember being before chronic fatigue became your new normal.
The technology exists, the treatments work, and your health insurance likely covers the costs. The only question remaining is: what are you waiting for?
For comprehensive sleep analysis and personalized snoring management strategies, SnailSleep provides professional-grade monitoring trusted by over 80 million users worldwide. Our advanced algorithms can help identify your specific snoring patterns and recommend evidence-based interventions tailored to your individual sleep profile.
References:
- Senaratna CV, et al. Prevalence of obstructive sleep apnea in the general population. Sleep Medicine Reviews. 2024;58:101-115.
- Chen X, et al. Racial/ethnic differences in sleep disturbances. Sleep Medicine. 2015;16(8):926-933.
- Young T, et al. Sleep disordered breathing and mortality: eighteen-year follow-up. Sleep. 2008;31(8):1071-1078.
- Peppard PE, et al. Increased prevalence of sleep-disordered breathing in adults. American Journal of Epidemiology. 2013;177(9):1006-1014.
- Gottlieb DJ, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure. Circulation. 2010;122(4):352-360.
- Marin JM, et al. Long-term cardiovascular outcomes in men with obstructive sleep apnea-hypopnea with or without treatment with CPAP. The Lancet. 2005;365(9464):1046-1053.
- Benjafield AV, et al. Estimation of the global prevalence and burden of obstructive sleep apnea. The Lancet Respiratory Medicine. 2019;7(8):687-698.
- Malhotra A, et al. Tirzepatide for the treatment of obstructive sleep apnea and obesity. New England Journal of Medicine. 2024;391(24):2307-2319.
Related Articles
- Obstructive Sleep Apnea Symptoms: Recognizing the Silent Threat to Your Health
- When Snoring Gets Dangerous: Early Warning Signs of Sleep Apnea
- Tracking Your Sleep with Technology: A Step-by-Step Guide