Unraveling the Nightly Symphony: A Comprehensive Guide to Snoring and Sleep Apnea
Snoring, often dismissed as a mere nocturnal nuisance, can be a significant indicator of underlying health issues. While it might seem like a harmless habit, understanding its mechanisms, causes, and potential health implications is crucial for both snorers and their bed partners. This comprehensive guide delves into the world of snoring, from its basic definition to advanced diagnostic methods and treatment options, aiming to provide clarity and empower individuals to seek appropriate care.
What is Snoring?
 Person snoring in bed
Person snoring in bed
Snoring is the harsh sound that occurs when air flow is obstructed through the nose and mouth during sleep. It is caused by the vibration of soft tissues in the upper airway, particularly the soft palate. The reason people don't snore when awake is that muscle tone, which is the sole component of vibration, changes during sleep. When we sleep, the muscles in our throat and tongue relax, leading to a narrowing of the airway. This narrowed passage, much like a flag fluttering in the wind, causes the soft tissues to vibrate as air passes through, producing the characteristic snoring sound. This phenomenon is exacerbated by increased local airflow velocity for a given inspiratory volume, which directly promotes vibration and further reduces intraluminal pressure, enhancing airway collapse and thus, snoring. Most snoring occurs during inspiration, though some can also occur during expiration.
How Common is Snoring?
Snoring is a widespread phenomenon, affecting a significant portion of the adult population. According to the May 2022 update of the Merck Manual, approximately 57% of men and 40% of women experience snoring, with its prevalence increasing with age. A 2021 study by Zhu Hua on snoring among university students in China revealed that 53.1% of male students and 29.9% of female students habitually snore. This percentage is observed to rise with advancing age, indicating a clear correlation between age and the likelihood of snoring.
What Causes Snoring?
Snoring can be attributed to a variety of physiological factors and lifestyle choices that contribute to the narrowing or obstruction of the upper airway during sleep. Understanding these causes is the first step towards effective management and treatment.
Physiological Factors:
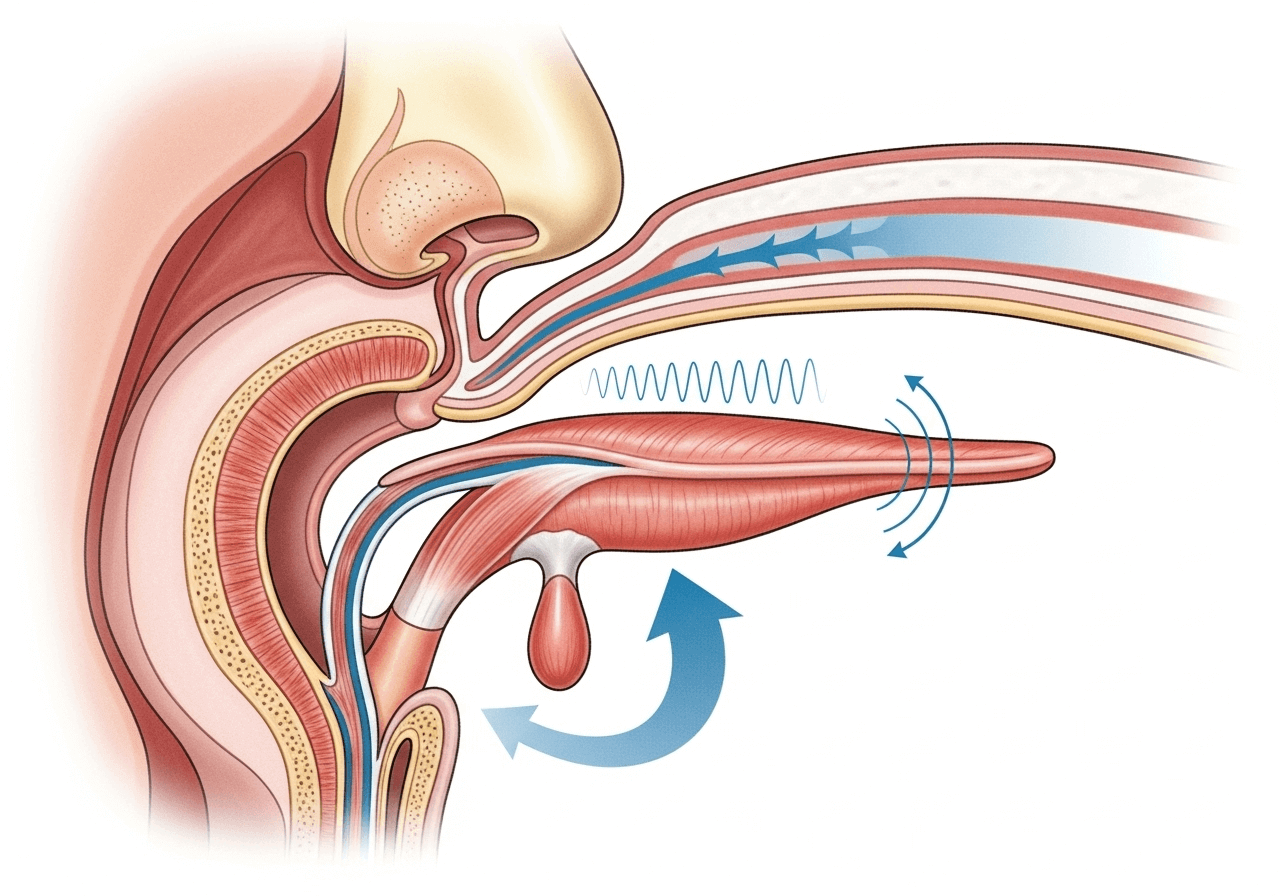 Medical illustration of upper airway
Medical illustration of upper airway
- Poor Muscle Tone in the Throat and Tongue: During sleep, the muscles in the throat and tongue can become overly relaxed, causing them to collapse into the airway and obstruct airflow.
- Nasal Airway Obstruction: Blockages in the nasal passages can force air to be inhaled through the mouth, increasing the likelihood of snoring. Common causes include:
- Deviated nasal septum (a displacement of the wall that divides the nostrils).
- Nasal polyps (soft, painless, noncancerous growths on the lining of your nasal passages or sinuses).
- Rhinitis (inflammation of the nasal lining) caused by allergies or sinus infections, leading to swollen tissues.
- Bulky Throat Tissue Due to Overweight/Obesity: Excess fatty tissue around the throat can narrow the airway.
- Small or Recessed Jaw: A smaller or backward-positioned jaw can reduce the space at the back of the throat.
- Long Soft Palate and/or Uvula: An elongated soft palate or uvula (the small, fleshy projection hanging at the back of the soft palate) can narrow the opening from the nose to the throat.
- Enlarged Tongue (Macroglossia): A larger than normal tongue can obstruct the airway.
- Enlarged Tonsils and Adenoids: These lymphatic tissues, especially common in children, can block the airway.
- Pregnancy: Hormonal changes and weight gain during pregnancy can contribute to snoring.
- Postmenopausal State: Hormonal shifts after menopause can affect muscle tone and contribute to snoring.
Lifestyle Factors:
- Alcohol Consumption or Sedative Use Before Bed: Alcohol and certain sedatives (like tranquilizers) can over-relax the throat and tongue muscles, increasing airway collapse.
- Sleep Position: Sleeping on your back can cause the tongue and soft palate to fall back into the throat, obstructing the airway. Using pillows that are too soft or too large can also contribute to snoring.
- Sleep Deprivation or Excessive Fatigue: When severely sleep-deprived or overly tired, throat muscles may relax excessively, leading to snoring.
When to Seek Medical Attention for Snoring?
While occasional, mild snoring is generally considered normal and does not require medical intervention, frequent or loud snoring can be a sign of a more serious underlying condition, such as obstructive sleep apnea (OSA). The primary impact of mild snoring might be limited to disturbing a bed partner; however, certain signs warrant a medical evaluation.
Primary snoring occurs more than three nights a week without associated awakenings, airflow limitation, oxygen desaturation, or arrhythmias during sleep, and without excessive daytime sleepiness. While more disruptive to bed partners due to its frequency, it is not typically considered a health concern unless there are signs of sleep disruption or sleep apnea, which would necessitate diagnostic testing.
You should pay special attention and consider consulting a doctor if you experience any of the following, as these may be potential signs of sleep apnea:
- Snoring occurring three or more nights per week.
- Very loud or bothersome snoring.
- Snoring accompanied by gasping, choking, or snorting sounds.
- Obesity or recent weight gain.
- Excessive daytime sleepiness.
- Difficulty concentrating or mental fogginess.
- Morning headaches and congestion.
- High blood pressure.
- Nighttime teeth grinding (bruxism).
- Frequent nighttime urination (nocturia).
From a health perspective, OSA-related snoring is of greater concern. Obstructive sleep apnea is diagnosed when a patient experiences five or more episodes of apnea or hypopnea (cessation or significant reduction in airflow) per hour during sleep (Apnea-Hypopnea Index [AHI]), coupled with one or more of the following:
- Daytime sleepiness, unintentional sleep episodes, unrefreshing sleep, fatigue, or insomnia.
- Waking up with gasping, choking, or snorting.
- Reported by a bed partner of loud snoring, breathing interruptions, or both during sleep.
Obstructive sleep apnea is classified by severity:
- Mild: 5 to 15 AHI events per hour.
- Moderate: 16 to 30 AHI events per hour.
- Severe: More than 30 AHI events per hour.
Upper Airway Resistance Syndrome (UARS), resulting from increased upper airway resistance or respiratory effort-related arousals (RERAs), can lead to excessive daytime sleepiness or other symptoms suggestive of OSA. However, it rarely involves apnea/hypopnea or oxygen desaturation, thus not meeting the full criteria for OSA.
Untreated OSA can significantly impact an individual's sleep and overall health. It is linked to dangerous daytime sleepiness and serious health conditions, including cardiovascular disease, hypertension, diabetes, stroke, and depression.
Which Department to Consult?
 Doctor consulting patient
Doctor consulting patient
Patients can typically consult an Ear, Nose, and Throat (ENT) specialist, an Oral and Maxillofacial surgeon, or a Pulmonologist. It is generally recommended to start with an ENT specialist to investigate the cause of snoring. If conditions like enlarged tonsils, deviated nasal septum, or nasal polyps are diagnosed, surgical treatment might be necessary.
If the issue is related to craniofacial problems, such as a small jaw (micrognathia), an Oral and Maxillofacial surgeon would be the appropriate specialist. For suspected sleep apnea or if there are co-existing chronic lung diseases, a Pulmonologist should be consulted for diagnosis and treatment.
How Do Doctors Examine Snoring?
When you consult a doctor for snoring, they will typically begin by taking a detailed medical history. This includes inquiring about the severity of your snoring, such as its frequency, duration, and loudness. The impact of snoring on your bed partner is also an important consideration.
Tools like the Epworth Sleepiness Scale and the STOP-BANG questionnaire (refer to the Obstructive Sleep Apnea Syndrome STOP-BANG Risk Score Table) are commonly used to assess the risk of OSA in snoring patients.
Your past medical history will also be reviewed for conditions potentially associated with OSA, particularly hypertension, coronary artery ischemia, heart failure, stroke, gastroesophageal reflux disease (GERD), atrial fibrillation, depression, obesity (especially morbid obesity), and diabetes. You will be asked about your alcohol consumption, including the amount and timing relative to bedtime. A review of your medication history will identify any sedative or muscle-relaxing drugs.
A physical examination will be conducted, starting with measurements of your height and weight to calculate your Body Mass Index (BMI). The rest of the examination will focus on your nose and mouth for signs of obstruction. These signs may include:
- Nasal polyps and congested turbinates.
- A high and narrow arched palate.
- Enlarged tongue, tonsils, soft palate, pharyngeal sidewalls, or uvula.
- A small or posteriorly displaced mandible (retrognathia).
Modified Mallampati Score of 3 or 4 (where only the base of the uvula or no uvula is visible during an oral examination, see Mallampati Score diagram) indicates an increased risk of OSA. The modified Mallampati classification is as follows:
- Class 1: Full visibility of the tonsils, uvula, and soft palate.
- Class 2: Visibility of the hard and soft palates, upper part of the tonsils, and uvula.
- Class 3: Visibility of the soft palate, hard palate, and base of the uvula.
- Class 4: Only the hard palate is visible.
Red Flags
The following findings are particularly concerning and warrant further investigation:
- Observed apneas or choking during sleep.
- Morning headaches.
- Epworth Sleepiness Scale score ≥ 10.
- BMI ≥ 35 kg/m².
- Very loud, persistent snoring.
- Hypertension.
Interpretation of Findings
Clinical assessment alone is not entirely reliable for diagnosing OSA but can be highly suggestive. The presence of red flags is strongly associated with OSA. However, these findings exist along a continuum, and there is no broad consensus on precise cutoff points or relative weights. Nevertheless, the more red flags a patient exhibits, the more severe the condition and the higher the likelihood of OSA.
Diagnostic Tests
Testing is performed when OSA is suspected and typically involves polysomnography (in-laboratory or home sleep study). However, given the high prevalence of snoring, polysomnography should only be performed when OSA is clinically suspected. A reasonable approach is to test patients with concerning findings (especially witnessed apneas) and those with multiple risk factors whose test scores (e.g., STOP-BANG risk score for OSA) are insufficient to diagnose OSA.
How to Treat Snoring? Advantages and Disadvantages of Various Therapies
Treatment for snoring generally involves managing risk factors through general measures and physical methods to open the airway and/or stiffen relevant structures.
General Measures
For primary snoring, several conventional measures can be employed. Their efficacy is not always well-evaluated, mainly because the perception of snoring is highly subjective; however, specific patients may benefit. Measures include:
- Avoiding alcohol and sedative medications several hours before bedtime.
- Sleeping with the head elevated (preferably using a bed or body positioning device, such as a wedge pillow).
- Sleeping on your side (e.g., using a specialized pillow like the 'Snail Dream Pillow').
- Weight loss (and oropharyngeal muscle training).
- Treating any nasal congestion:
- Using decongestants and/or corticosteroid nasal sprays (e.g., referencing Matsukiyo or similar allergy nasal sprays).
- Taking a hot shower before bed to reduce nasal congestion.
- Maintaining a saline rinse bottle (e.g., referencing NeilMed).
- Using internal nasal dilators during sleep (e.g., referencing WoodyKnows, Rhinomed limited edition silent nasal dilators).
Bed partners may benefit from using earplugs (e.g., Mack's Pillow Soft Silicone Earplugs, 22 dB noise reduction; Flents Ear Plugs, 10 pairs with case, 33 dB noise reduction) or white noise devices. Sometimes, alternating sleep arrangements (e.g., separate rooms) may be necessary.
Oral Appliances
Oral appliances are worn only during sleep and include:
- Mandibular Advancement Devices (MADs): These are the most commonly used. They move the lower jaw and tongue forward relative to the upper jaw, thereby increasing the airway caliber during sleep. These devices can be incrementally adjusted after initial fitting to optimize results.
- Tongue Retaining Devices (TRDs): These devices use suction to hold the tongue in a forward position. TRDs are generally less comfortable than MADs.
These devices must be fitted by a specially trained dentist. They are helpful for OSA patients and are generally considered effective for simple snoring, although research in this area is limited. Side effects may include temporomandibular joint (TMJ) discomfort, tooth misalignment, and excessive salivation, but most patients tolerate the devices well.
Continuous Positive Airway Pressure (CPAP) and Bi-level Positive Airway Pressure (BiPAP)
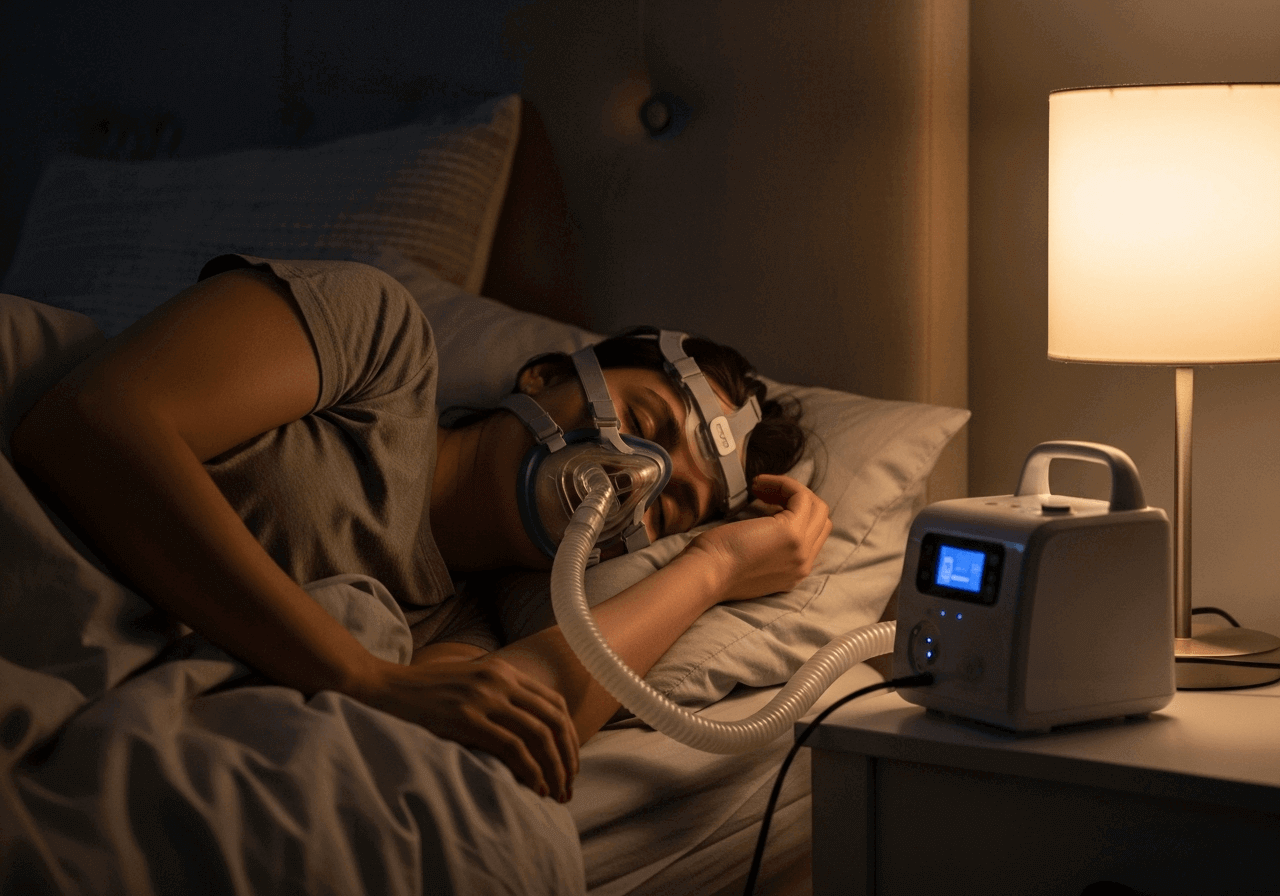 Person using CPAP machine
Person using CPAP machine
CPAP devices maintain a constant positive pressure in the upper airway through a small mask worn over the nose or nose and mouth. By increasing the upper airway's caliber, CPAP prevents the upper airway from narrowing or collapsing during sleep. Therefore, it is highly effective for OSA and also effective for primary snoring. However, its use in primary snoring is limited due to a lack of third-party reimbursement. While patients are generally willing to use CPAP devices nightly to avoid the significant symptoms and long-term consequences of OSA, they are less willing to use the device for primary snoring, which is primarily a social issue.
Surgical Interventions
Since reduced nasal patency can promote snoring, surgical correction of specific causes of airway impairment (e.g., nasal polyps, enlarged tonsils, deviated nasal septum) can be a reasonable approach to reduce snoring. However, research has not consistently confirmed this theory.
Various pharyngeal surgeries that alter the structure of the palate, and sometimes the uvula, have been developed to treat obstructive sleep apnea. Some are also useful for non-apneic snoring.
- Uvulopalatopharyngoplasty (UPPP): This procedure involves reconstructing the uvula, palate, and pharyngeal walls to increase the size of the airway. It can be effective for snoring, although the effects may not last for more than a few years. This is an inpatient procedure requiring general anesthesia; therefore, its role for snoring alone is limited.
Consequently, several outpatient palatal modification procedures requiring only local anesthesia have been developed:
- Laser-Assisted Uvulopalatoplasty (LAUP): Less invasive than UPPP. While some patients report benefits, its role in treating snoring has not been definitively established.
- Injection Snoreplasty: Involves injecting a sclerosing agent into the submucosal layer of the soft palate to stiffen the soft palate and uvula. Its effect on snoring requires further study.
- Radiofrequency Ablation (RFA): Uses a probe to deliver thermal energy to the soft palate. Studies suggest it can be useful for snoring, but further research is needed.
- Palatal Implants: Small implants made of polyethylene can be placed in the soft palate to stiffen it. Three small implants are typically used. Their use for snoring alone has not been definitively proven, and these implants can sometimes extrude.
Key Takeaways
- Only some snorers have obstructive sleep apnea (OSA), but most OSA patients snore.
- Clinical risk factors, such as witnessed apneas or choking episodes during sleep, daytime sleepiness, and high BMI, help identify patients at risk for OSA, thus necessitating polysomnography or home sleep studies.
- General measures to reduce snoring are recommended.
- Specific measures, such as mandibular advancement devices, uvulopalatopharyngoplasty, palatal modification procedures, and CPAP, should be considered for OSA-related snoring.
Modified Mallampati Score Classification
| Class | Description |
|---|---|
| Class 1 | Full visibility of the tonsils, uvula, and soft palate. |
| Class 2 | Visibility of the hard and soft palates, upper part of the tonsils, and uvula. |
| Class 3 | Visibility of the soft palate, hard palate, and base of the uvula. |
| Class 4 | Only the hard palate is visible. |
Note: The STOP-BANG questionnaire is another commonly used tool for assessing the risk of Obstructive Sleep Apnea (OSA).
STOP-BANG Questionnaire
The STOP-BANG questionnaire is a widely used screening tool for assessing the risk of Obstructive Sleep Apnea (OSA). It consists of eight yes/no questions, with one point awarded for each 'yes' answer. The total score helps categorize the risk of OSA.
| Question | Yes/No |
|---|---|
| Snore: Do you snore loudly (louder than talking or almost always snore)? | |
| Tired: Do you often feel tired, fatigued, or sleepy during the daytime (e.g., falling asleep while driving or talking)? | |
| Observed: Has anyone observed you stop breathing, choke, or gasp during your sleep? | |
| Pressure: Do you have or are you being treated for high blood pressure? | |
| BMI: Is your Body Mass Index (BMI) greater than 27 kg/m²? | |
| Age: Are you older than 50 years old? | |
| Neck circumference: Is your neck circumference greater than 16 inches (40 cm)? | |
| Gender: Are you male? |
Interpretation of STOP-BANG Score:
-
Low Risk of OSA: 0-2 'Yes' answers
-
Intermediate Risk of OSA: 3-4 'Yes' answers
-
High Risk of OSA: 5-8 'Yes' answers
Alternatively, High Risk is also considered if you answer 'Yes' to 2 or more of the STOP questions (Snoring, Tired, Observed Apnea, Blood Pressure) AND your BMI is > 27 kg/m², OR your neck circumference is > 40 cm, OR you are male.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Please consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Responsive Design Note
This document is formatted using Markdown, which inherently supports responsive design principles. The content will adapt to various screen sizes (desktop, mobile, tablet) for optimal readability. Images are included with relative paths, allowing them to scale appropriately within the viewing environment.
Related Articles
- Obstructive Sleep Apnea Symptoms: Recognizing the Silent Threat to Your Health
- When Snoring Gets Dangerous: Early Warning Signs of Sleep Apnea
- Light Snoring vs. Sleep Apnea: Why It Matters More Than You Think
