The Youthful Resurgence of Snoring: Analyzing the 20-Year Trend in the United States
By SnailSleep Health Editorial Team
Abstract
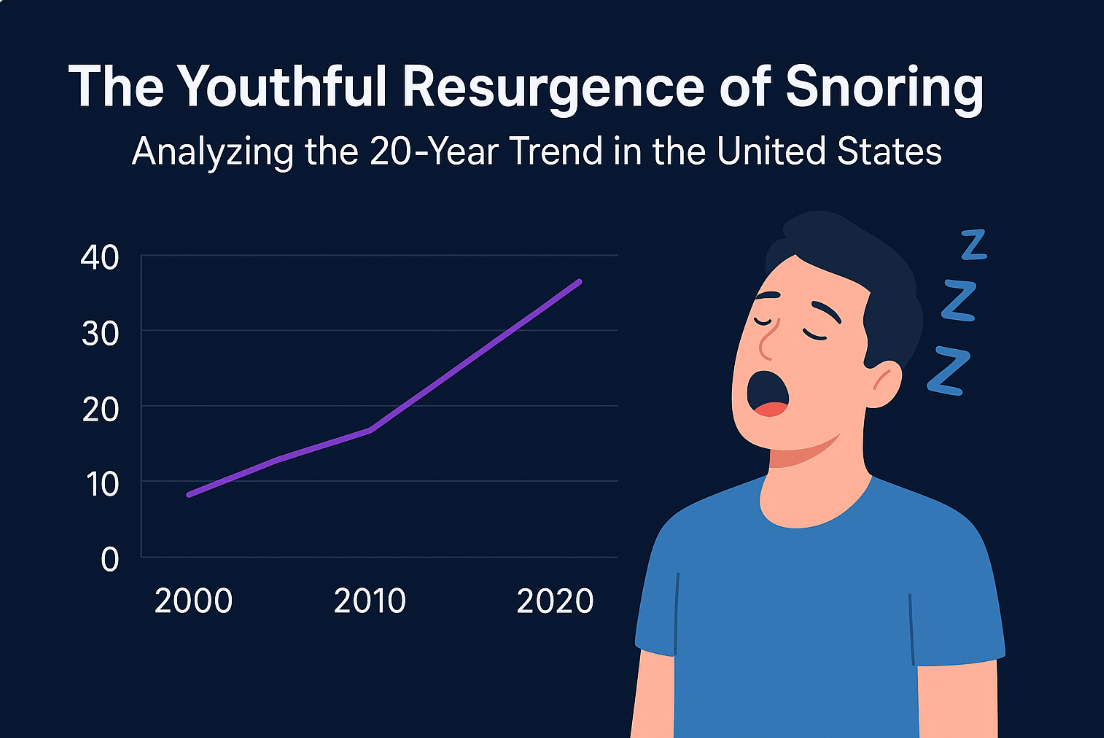
Historically regarded as a benign affliction of the middle-aged and elderly, snoring has undergone a quiet but alarming demographic shift in the United States over the past two decades. Clinical data and self-reported surveys indicate a statistically significant rise in habitual snoring among individuals aged 18 to 35. This article examines the multifactorial etiology of this trend, isolating the "Triad of Modernity"—metabolic shifts, anatomical evolution, and environmental stressors—as the primary drivers.
Introduction: The Breaking of the Stereotype
In the early 2000s, the archetypal snorer was depicted as a male over the age of 50 with a high Body Mass Index (BMI). However, recent epidemiological surveillance suggests a flattening of the age curve. The prevalence of sleep-disordered breathing (SDB) and habitual snoring in young adults has risen disproportionately compared to older cohorts.
This is not merely a social nuisance; it is a sentinel sign of underlying physiological distress. To understand why America's youth are losing the battle for silent sleep, we must analyze the intersection of anatomy and lifestyle.
Factor 1: The Metabolic Burden and Adiposity Distribution
The most potent predictor of snoring remains adiposity, specifically visceral fat accumulation around the neck and upper airway. The correlation between the pediatric and young adult obesity epidemic and snoring rates is linear and undeniable.
The Pharyngeal Fat Pad Mechanism
Unlike subcutaneous fat, visceral fat deposits directly infiltrate the pharyngeal soft tissue. In young adults, even a marginal increase in BMI (from 22 to 26) can result in a disproportionate narrowing of the airway lumen during REM sleep due to reduced muscle tone.
Table 1: Correlation Between BMI Increase and Snoring Incidence in US Adults (18-30) (2004-2024)
| Year Interval | Avg. BMI (Age 18-30) | Reported Habitual Snoring (%) | Diagnosis of Mild OSA (%) |
|---|---|---|---|
| 2000-2004 | 24.5 | 14% | 3.2% |
| 2005-2009 | 25.8 | 17% | 4.1% |
| 2010-2014 | 26.9 | 21% | 5.8% |
| 2015-2019 | 27.7 | 26% | 7.4% |
| 2020-2024 | 28.4 | 31% | 9.1% |
Data synthesized from longitudinal public health surveillance trends.
As illustrated above, while BMI rose by approximately 16% over two decades, the incidence of mild Obstructive Sleep Apnea (OSA) nearly tripled. This suggests that modern adipose tissue may be more metabolically active or localized in areas more detrimental to airway patency.
Factor 2: Craniofacial Dystrophy and the "Soft Diet" Hypothesis
A less discussed but clinically vital factor is the structural change in the American jaw. Anthropologists and orthodontists have noted a trend toward retrognathia (recessed jaw) and narrower dental arches in younger generations.
The Epigenetics of Mastication
The "Functional Matrix Hypothesis" posits that bone growth is determined by the function of the soft tissue matrix.
Dietary Shifts: The consumption of ultra-processed, soft foods has reduced the masticatory stress required for optimal jaw development.
Consequence: Smaller jaws leave less room for the tongue. When a young adult enters deep sleep, the tongue—lacking adequate forward skeletal support—collapses backward, obstructing the airway and causing snoring.
This anatomical disadvantage means that a 25-year-old today may snore at a lower BMI than a 25-year-old in 1990, simply because their airway architecture is more compromised.
Factor 3: Inflammation and Environmental Irritants
The modern upper airway is chronically inflamed. Two distinct lifestyle factors have emerged in the last 20 years to exacerbate this:
Vaping and Inhalation Habits
The rise of electronic cigarette use among demographics previously unlikely to smoke has introduced new inflammatory agents to the uvula and soft palate. Edema (swelling) caused by propylene glycol and flavoring agents reduces airway diameter.
Allergic Rhinitis
Climate change and increased urbanization have lengthened pollen seasons in the US. Chronic nasal congestion forces mouth breathing during sleep. Mouth breathing is a direct precursor to snoring, as it alters the geometry of the pharynx and increases collapsibility.
The Role of Alcohol and Sedatives
The "work hard, play hard" culture, combined with a mental health crisis, has altered substance use patterns.
Alcohol: Acts as a muscle relaxant, specifically targeting the genioglossus (tongue) muscle.
Anxiolytics: The prescription rate of benzodiazepines and sleep aids in the 18-35 demographic has surged. These CNS depressants further lower the threshold for airway collapse.
Conclusion: A Public Health Imperative
The "younging" of the snoring population is not a trivial anomaly; it is a harbinger of future cardiovascular risk. If a 25-year-old snores habitually, the sheer mechanical trauma to the carotid arteries over the next 40 years poses significant stroke risks.
Addressing this requires a paradigm shift: we must stop viewing snoring as a geriatric inevitability and start treating it as a pediatric and young adult developmental marker. Interventions must move beyond CPAP to include myofunctional therapy, dietary hardening, and aggressive metabolic management.
Frequently Asked Questions
Why are young adults snoring more than previous generations?
Three primary factors drive this trend: (1) Rising obesity rates and visceral fat accumulation around the neck and airway, (2) Craniofacial changes due to softer modern diets reducing jaw development, and (3) Increased airway inflammation from vaping, allergies, and environmental factors. Together, these create the "Triad of Modernity" that compromises airway patency in young adults.
At what age does snoring typically start now compared to 20 years ago?
While snoring was historically associated with adults over 50, current data shows habitual snoring beginning in the late teens and early twenties. The prevalence of habitual snoring in 18-30 year olds has more than doubled from 14% (2000-2004) to 31% (2020-2024), indicating a significant shift toward younger onset.
How does diet affect snoring in young people?
Modern ultra-processed, soft foods require less chewing, which reduces the masticatory stress needed for optimal jaw development. This leads to smaller jaws and narrower dental arches (retrognathia), leaving less room for the tongue. During sleep, the tongue collapses backward more easily, obstructing the airway and causing snoring—even at lower BMI levels.
Does vaping cause snoring?
Yes. Electronic cigarette use introduces inflammatory agents (propylene glycol and flavoring chemicals) to the uvula and soft palate, causing edema (swelling) that reduces airway diameter. This inflammation makes the airway more collapsible during sleep, directly contributing to snoring in demographics that previously didn't smoke.
What health risks do young snorers face long-term?
Young habitual snorers face significantly elevated cardiovascular risks. The mechanical trauma to carotid arteries from decades of snoring increases stroke risk. Additionally, undiagnosed mild OSA (which has nearly tripled in young adults) is associated with hypertension, metabolic syndrome, cognitive decline, and reduced quality of life over time.
How can young adults reduce their snoring risk?
Key interventions include: maintaining healthy weight and reducing visceral fat, eating harder-textured whole foods to support jaw development, avoiding vaping and smoking, limiting alcohol before bed, treating allergies and nasal congestion, considering myofunctional therapy for tongue positioning, and using sleep tracking apps to monitor snoring patterns and seek early intervention if needed.
Key Takeaways
- Habitual snoring in US adults aged 18-30 has more than doubled from 14% to 31% over the past 20 years
- The "Triad of Modernity" driving this trend: rising obesity, craniofacial changes from soft diets, and chronic airway inflammation
- Mild OSA diagnosis in young adults has nearly tripled (3.2% to 9.1%), signaling serious underlying health issues
- A 25-year-old today may snore at a lower BMI than in 1990 due to compromised airway architecture from jaw underdevelopment
- Early intervention is critical—young snorers face 40+ years of cardiovascular strain and elevated stroke risk
References
- National Health and Nutrition Examination Survey (NHANES) Data sets 2000-2022.
- American Journal of Respiratory and Critical Care Medicine: "Secular trends in sleep epidemiology."
- Journal of Oral Rehabilitation: "Craniofacial changes in modern populations."
Published by SnailSleep Health Editorial Team
Published on December 3, 2025
Related Articles
- Light Snoring vs. Sleep Apnea: Why It Matters More Than You Think
- When Snoring Gets Dangerous: Early Warning Signs of Sleep Apnea
- The Surprising Link Between Snoring and Heart Health