Oral Appliances: Non-CPAP Sleep Apnea Treatment Options
Published by Dr. Sarah Thompson | Sleep Research Director
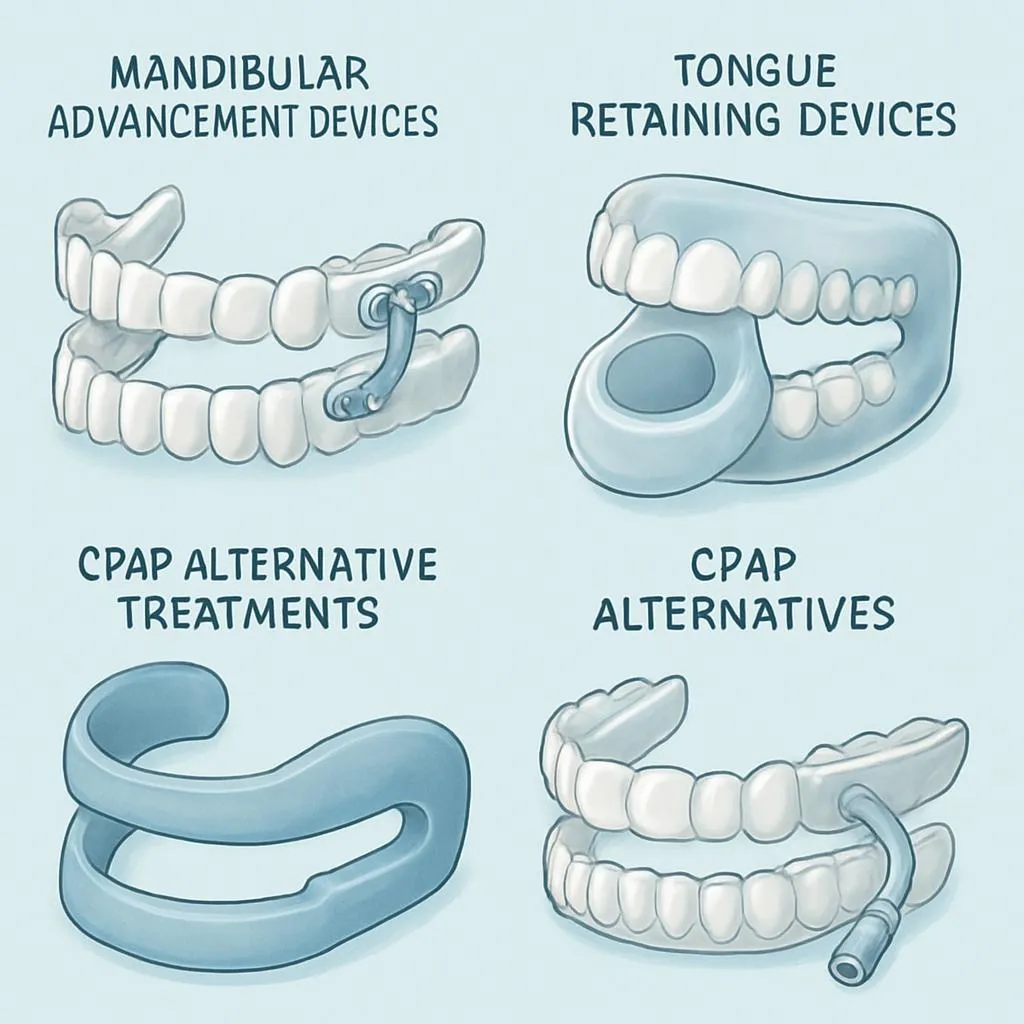 Oral Appliances: Non-CPAP Sleep Apnea Treatment Options illustration
Oral Appliances: Non-CPAP Sleep Apnea Treatment Options illustration
Narcolepsy is far more than just feeling unusually tired during the day. This neurological disorder affects approximately 200,000 Americans and can significantly impact daily functioning, work performance, and quality of life. Understanding the difference between normal fatigue and narcolepsy symptoms is crucial for proper diagnosis and treatment.
Understanding Oral Appliances
This condition represents a significant aspect of sleep health that affects millions of people worldwide. Understanding its mechanisms, symptoms, and treatment options is crucial for anyone experiencing sleep-related challenges.
Definition and Scope
Alternative treatments for sleep apnea using oral devices. This comprehensive overview will explore evidence-based approaches to understanding and managing this condition effectively.
Prevalence and Impact
Sleep disorders affect approximately 50-70 million Americans, with this particular condition representing a substantial portion of sleep-related health concerns. The impact extends beyond just nighttime symptoms, affecting daytime functioning, quality of life, and overall health outcomes.
The Science Behind the Condition
Neurobiological Mechanisms
Research has identified several key mechanisms underlying this condition:
Brain Chemistry and Neurotransmitters:
- Sleep-wake regulation involves complex interactions between multiple neurotransmitter systems
- Disruptions in these systems can lead to various sleep disorders
- Understanding these mechanisms helps guide effective treatment approaches
Circadian Rhythm Involvement:
- The body's internal clock plays a crucial role in sleep timing and quality
- Disruptions to circadian rhythms can exacerbate sleep problems
- Light exposure, meal timing, and sleep schedule all influence circadian function
Genetic Factors:
- Many sleep disorders have hereditary components
- Genetic variations can affect sleep architecture and disorder susceptibility
- Family history often provides important diagnostic clues
Current Research Findings
Recent studies have revealed important insights into sleep disorder mechanisms:
- Advanced brain imaging shows specific neural pathway disruptions
- Genetic research identifies susceptibility markers
- Treatment response studies guide personalized therapy approaches
Signs and Symptoms to Watch For
Primary Symptoms to Monitor
Sleep-Related Symptoms:
- Difficulty falling asleep or staying asleep
- Frequent awakenings during the night
- Non-restorative sleep despite adequate time in bed
- Changes in normal sleep patterns or timing
Daytime Symptoms:
- Excessive daytime fatigue or sleepiness
- Difficulty concentrating or remembering information
- Mood changes including irritability or depression
- Reduced performance at work or school
Physical Symptoms:
- Morning headaches or feeling unrefreshed
- Physical discomfort or pain affecting sleep
- Changes in appetite or weight
- Increased susceptibility to illness
When to Seek Professional Help
Consider consulting a healthcare provider if symptoms:
- Persist for more than 2-3 weeks despite good sleep hygiene
- Significantly impact daily functioning or quality of life
- Are accompanied by concerning physical symptoms
- Affect relationships or work performance
Causes and Contributing Factors
Primary Risk Factors
Genetic Predisposition:
- Family history significantly increases risk
- Specific genetic markers associated with sleep disorders
- Inherited variations in sleep-related neurotransmitter function
- Environmental factors may trigger genetic susceptibility
Lifestyle Factors:
- Irregular sleep schedules and poor sleep hygiene
- High stress levels and inadequate stress management
- Excessive caffeine, alcohol, or nicotine consumption
- Lack of regular physical exercise
Medical Conditions:
- Neurological disorders affecting sleep centers
- Hormonal imbalances and endocrine disorders
- Respiratory conditions affecting breathing during sleep
- Mental health conditions including anxiety and depression
Environmental Influences:
- Shift work or frequent travel across time zones
- Exposure to excessive light or noise during sleep hours
- Uncomfortable sleep environment (temperature, bedding)
- Life changes or traumatic events affecting sleep patterns
Age and Gender Considerations
- Certain sleep disorders are more common in specific age groups
- Hormonal changes during puberty, pregnancy, or menopause can trigger symptoms
- Men and women may experience different symptom patterns
- Aging naturally affects sleep architecture and disorder susceptibility
Treatment Options and Management Strategies
Medical Treatment Options
Pharmacological Interventions:
- Prescription medications targeting specific neurotransmitter systems
- Sleep aids for short-term symptom relief
- Medications to address underlying medical conditions
- Regular monitoring for effectiveness and side effects
Behavioral Therapies:
- Cognitive Behavioral Therapy for Insomnia (CBT-I)
- Sleep restriction therapy to improve sleep efficiency
- Stimulus control techniques to strengthen sleep associations
- Relaxation training and stress management techniques
Medical Devices and Equipment:
- CPAP machines for breathing-related sleep disorders
- Oral appliances for sleep apnea and bruxism
- Light therapy boxes for circadian rhythm disorders
- Specialized pillows or positional therapy devices
Professional Sleep Medicine Evaluation
Sleep Study Options:
- Overnight polysomnography (PSG) in sleep centers
- Home sleep apnea testing for specific conditions
- Multiple Sleep Latency Test (MSLT) for excessive sleepiness
- Maintenance of Wakefulness Test (MWT) for safety-critical occupations
Diagnostic Procedures:
- Comprehensive medical and sleep history review
- Physical examination focusing on sleep-related factors
- Laboratory tests to rule out underlying medical conditions
- Neurological evaluation when indicated
Lifestyle Changes for Better Sleep Health
Sleep Hygiene Optimization
Bedroom Environment:
- Maintain cool temperature (60-67°F) for optimal sleep
- Ensure complete darkness with blackout curtains or eye masks
- Minimize noise with earplugs or white noise machines
- Invest in comfortable, supportive mattress and pillows
Daily Routine Modifications:
- Establish consistent sleep and wake times, even on weekends
- Create a relaxing 1-2 hour wind-down routine before bed
- Limit screen exposure 1 hour before bedtime
- Practice relaxation techniques such as deep breathing or meditation
Dietary Considerations:
- Avoid large meals, caffeine, and alcohol close to bedtime
- Consider sleep-promoting foods like tart cherries or warm milk
- Stay hydrated throughout the day but limit fluids before bed
- Maintain regular meal times to support circadian rhythm
Stress Management Strategies
Relaxation Techniques:
- Progressive muscle relaxation for physical tension relief
- Mindfulness meditation to calm racing thoughts
- Journaling to process daily concerns before bed
- Gentle yoga or stretching to prepare the body for sleep
Cognitive Strategies:
- Worry time designation earlier in the evening
- Positive visualization and guided imagery
- Gratitude practice to shift focus from stressors
- Problem-solving techniques to address underlying concerns
Prevention and Long-term Success
Prevention Strategies
Early Intervention:
- Recognize warning signs before symptoms become severe
- Address lifestyle factors that may contribute to sleep problems
- Seek professional help at the first sign of persistent sleep issues
- Maintain regular health check-ups to monitor sleep health
Long-term Maintenance:
- Continue proven strategies even after symptoms improve
- Regular follow-up with healthcare providers as needed
- Adjust treatment approaches as life circumstances change
- Stay informed about new research and treatment options
Risk Factor Management:
- Maintain healthy weight through diet and exercise
- Manage stress through proven techniques and support systems
- Avoid substances that can disrupt sleep quality
- Create stable routines that support healthy sleep patterns
Building Sustainable Habits
Gradual Implementation:
- Start with one or two changes rather than overhauling everything
- Track progress to identify what works best for your situation
- Be patient as sleep improvements often take several weeks
- Celebrate small victories to maintain motivation
Support Systems:
- Involve family members in creating a sleep-friendly environment
- Consider joining support groups for specific sleep disorders
- Work with healthcare providers to develop personalized strategies
- Use technology tools to track progress and maintain accountability
Using Technology for Better Sleep Tracking
Sleep Tracking and Monitoring
SnailSleep App Features:
- Comprehensive sleep pattern analysis and reporting
- Audio monitoring to detect snoring and breathing irregularities
- Sleep stage tracking to understand sleep architecture
- Environmental factor correlation with sleep quality
Data-Driven Insights:
- Personalized recommendations based on individual patterns
- Trend analysis to identify improvement or concerning changes
- Correlation tracking between lifestyle factors and sleep quality
- Preparation for medical consultations with objective data
Smart Features for Better Sleep:
- Intelligent alarm timing during lighter sleep phases
- Customizable soundscapes for relaxation and sleep induction
- Progress tracking and goal setting for sleep improvement
- Integration with other health monitoring devices
Professional Integration
Healthcare Provider Collaboration:
- Detailed sleep reports for medical consultations
- Audio recordings of concerning breathing patterns
- Long-term trend data for diagnosis and treatment monitoring
- Treatment effectiveness tracking over time
Research Participation:
- Anonymous data contribution to sleep research studies
- Access to cutting-edge sleep health insights
- Participation in clinical trials and research opportunities
- Contributing to advancement of sleep medicine
Future Technology Developments
The field of sleep technology continues to evolve rapidly, with new innovations in artificial intelligence, wearable devices, and personalized medicine promising even more effective tools for sleep health management. SnailSleep remains at the forefront of these developments, continuously improving its capabilities to serve users' sleep health needs.
Conclusion
Understanding and addressing oral appliances: non-cpap sleep apnea treatment options is crucial for optimal sleep health and overall well-being. The evidence clearly shows that with proper knowledge, appropriate treatment, and consistent lifestyle modifications, significant improvement is possible for most individuals experiencing these challenges.
Key takeaways from this comprehensive guide include:
- Early recognition and intervention lead to better outcomes and prevent complications
- Professional medical evaluation is essential for proper diagnosis and treatment planning
- Lifestyle modifications play a crucial role in both treatment and prevention
- Technology tools like SnailSleep can provide valuable insights and support your health journey
- Consistency and patience are essential, as sleep improvements often take time to develop
Remember that sleep health is an investment in your overall quality of life. Quality sleep affects every aspect of your health, from cognitive function and emotional regulation to immune system strength and cardiovascular health. By taking proactive steps to address sleep concerns, you're making a commitment to your long-term health and well-being.
If you're experiencing persistent sleep problems, don't hesitate to seek professional help. Sleep disorders are medical conditions that deserve proper attention and treatment. With the right approach, support, and tools, you can achieve the restorative sleep your body and mind need to function at their best.
Start your journey to better sleep tonight by implementing one or two strategies from this guide. Track your progress with SnailSleep's comprehensive monitoring features, and remember that small, consistent changes often lead to the most sustainable improvements in sleep quality and overall health.
Keywords: oral appliances, sleep apnea treatment, CPAP alternatives, dental devices
For comprehensive sleep monitoring and personalized insights, download the SnailSleep app today.
Related Articles
- Sleep Apnea Treatment Options: From CPAP to Lifestyle Changes
- Sleep Apnea Solutions: Natural Treatment & Lifestyle Changes
- Sleep Apnea and Weight Management: A Critical Link to Better Sleep and Health
