Sleep Apnea and Weight Management: A Critical Link to Better Sleep and Health
Published by Dr. Jennifer Chen | Sleep Medicine and Weight Management Specialist
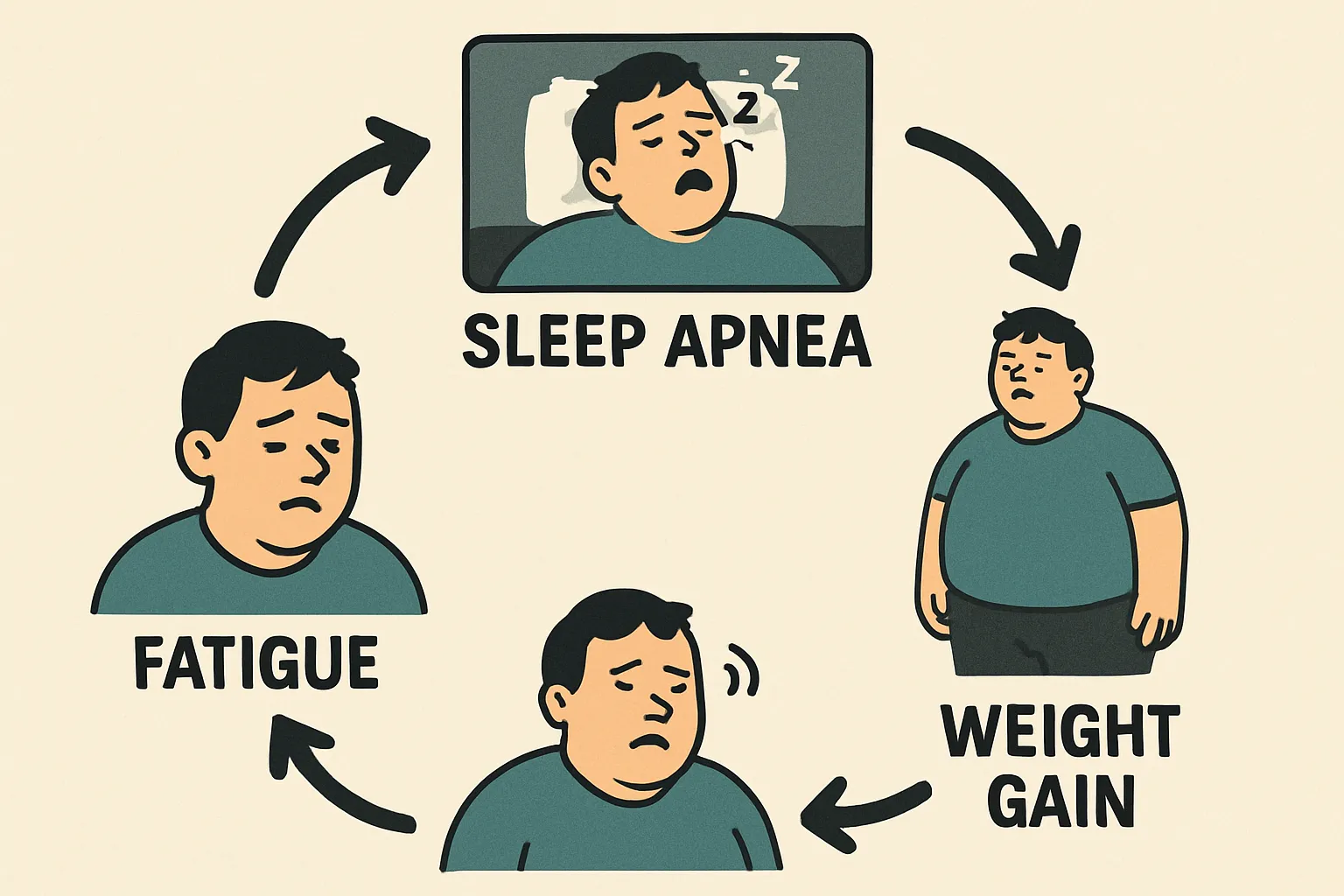 Sleep apnea obesity vicious cycle
Sleep apnea obesity vicious cycle
The relationship between sleep apnea and weight management is one of the most important yet often misunderstood connections in sleep medicine. This bidirectional relationship creates a vicious cycle where sleep apnea contributes to weight gain, and excess weight worsens sleep apnea symptoms. Understanding this connection is crucial for effective treatment and long-term health improvement. This comprehensive guide explores the science behind this relationship and provides practical strategies for breaking the cycle.
The Sleep Apnea-Weight Connection
Understanding the Bidirectional Relationship
Sleep Apnea → Weight Gain:
- Hormonal disruption: Sleep apnea affects leptin and ghrelin production
- Metabolic changes: Reduced insulin sensitivity and glucose metabolism
- Energy expenditure: Lower physical activity due to daytime fatigue
- Stress response: Elevated cortisol levels promote fat storage
Weight Gain → Sleep Apnea:
- Airway narrowing: Excess fat around neck constricts airway
- Tissue compression: Increased pressure on breathing passages
- Inflammation: Fat tissue produces inflammatory chemicals
- Muscle function: Reduced muscle tone in airway structures
 Weight management strategies for OSA
Weight management strategies for OSA
The Vicious Cycle Explained
Stage 1: Initial Weight Gain
- Lifestyle factors: Poor diet, lack of exercise, stress
- Medical conditions: Hypothyroidism, medications, hormonal changes
- Sleep disruption: Poor sleep quality affects metabolism
- Gradual progression: Weight increases slowly over time
Stage 2: Sleep Apnea Development
- Airway changes: Excess weight narrows breathing passages
- Sleep fragmentation: Breathing pauses disrupt sleep architecture
- Oxygen deprivation: Reduced oxygen levels during sleep
- Symptom onset: Snoring, breathing pauses, daytime fatigue
Stage 3: Worsening Cycle
- Metabolic disruption: Sleep apnea affects hormone production
- Increased appetite: Higher ghrelin, lower leptin levels
- Reduced activity: Daytime sleepiness limits exercise
- Further weight gain: Additional fat worsens sleep apnea
Stage 4: Health Complications
- Cardiovascular disease: High blood pressure, heart problems
- Diabetes: Insulin resistance and poor glucose control
- Metabolic syndrome: Cluster of health risk factors
- Quality of life: Significant impact on daily functioning
Scientific Evidence
Research Studies
Weight Loss Benefits:
- 10% weight loss: Can reduce AHI by 30-50%
- 20% weight loss: May eliminate sleep apnea in some cases
- Long-term studies: Sustained weight loss maintains improvements
- Combination therapy: Weight loss + CPAP more effective than either alone
Sleep Apnea Impact on Weight:
- Hormonal changes: Disrupted leptin and ghrelin production
- Metabolic rate: Reduced resting energy expenditure
- Physical activity: Lower exercise capacity and motivation
- Appetite regulation: Increased hunger and food cravings
 Weight loss improves sleep apnea
Weight loss improves sleep apnea
Hormonal Mechanisms
Leptin (Satiety Hormone):
- Normal function: Signals fullness and reduces appetite
- Sleep apnea effect: Reduced production and sensitivity
- Result: Increased hunger and reduced satiety
- Treatment response: Improves with sleep apnea treatment
Ghrelin (Hunger Hormone):
- Normal function: Stimulates appetite and food intake
- Sleep apnea effect: Elevated levels
- Result: Increased hunger and food cravings
- Treatment response: Decreases with sleep apnea improvement
Cortisol (Stress Hormone):
- Normal function: Regulates metabolism and stress response
- Sleep apnea effect: Elevated levels, especially at night
- Result: Increased fat storage, especially around abdomen
- Treatment response: Normalizes with sleep apnea treatment
Insulin:
- Normal function: Regulates blood sugar and fat storage
- Sleep apnea effect: Reduced sensitivity and production
- Result: Poor glucose control and increased fat storage
- Treatment response: Improves with weight loss and sleep apnea treatment
Weight Management Strategies for Sleep Apnea
Dietary Approaches
Calorie Control:
- Caloric deficit: 500-1000 calories below maintenance needs
- Macronutrient balance: 40% carbs, 30% protein, 30% fat
- Meal timing: Regular meals, avoid eating close to bedtime
- Portion control: Use smaller plates, measure portions
Specific Dietary Patterns:
- Mediterranean diet: Rich in vegetables, fruits, whole grains, lean protein
- Low-carb diets: May help with insulin resistance
- Intermittent fasting: Time-restricted eating patterns
- Plant-based diets: High fiber, low calorie density
Food Choices:
- High-fiber foods: Vegetables, fruits, whole grains, legumes
- Lean protein: Fish, poultry, lean meat, eggs, dairy
- Healthy fats: Nuts, seeds, olive oil, avocado
- Limit processed foods: High in calories, low in nutrients
Exercise Programs
Aerobic Exercise:
- Frequency: 3-5 times per week
- Duration: 30-60 minutes per session
- Intensity: Moderate to vigorous (60-80% max heart rate)
- Types: Walking, cycling, swimming, elliptical training
Strength Training:
- Frequency: 2-3 times per week
- Sets and reps: 2-3 sets of 8-12 repetitions
- Muscle groups: Major muscle groups, full body workouts
- Benefits: Increased muscle mass, improved metabolism
Flexibility and Balance:
- Yoga: Improves flexibility, reduces stress
- Tai chi: Gentle movement, balance training
- Stretching: Daily stretching routine
- Core exercises: Strengthen abdominal and back muscles
Behavioral Strategies
Goal Setting:
- Realistic targets: 1-2 pounds per week weight loss
- Short-term goals: Weekly and monthly targets
- Long-term vision: Ultimate weight and health goals
- Progress tracking: Regular weigh-ins and measurements
Self-Monitoring:
- Food diary: Record all food and beverage intake
- Activity tracking: Monitor exercise and daily movement
- Sleep diary: Track sleep quality and apnea symptoms
- Progress photos: Visual record of changes
Stress Management:
- Relaxation techniques: Deep breathing, meditation, progressive muscle relaxation
- Time management: Prioritize sleep, exercise, and healthy eating
- Social support: Family, friends, support groups
- Professional help: Counseling, therapy if needed
Breaking the Vicious Cycle
Step-by-Step Approach
Phase 1: Assessment and Planning (Weeks 1-2)
- Medical evaluation: Comprehensive health assessment
- Sleep study: Confirm sleep apnea diagnosis and severity
- Goal setting: Establish realistic weight loss targets
- Baseline measurements: Weight, body composition, sleep quality
Phase 2: Initial Changes (Weeks 3-8)
- Diet modifications: Implement calorie-controlled eating plan
- Exercise introduction: Begin with walking, gradually increase intensity
- Sleep optimization: Improve sleep hygiene and environment
- CPAP initiation: Begin sleep apnea treatment if prescribed
Phase 3: Building Habits (Weeks 9-16)
- Routine establishment: Consistent eating and exercise schedules
- Progress monitoring: Regular assessment of weight and sleep
- Habit formation: Sustainable lifestyle changes
- Social support: Engage family and friends in the process
Phase 4: Maintenance (Weeks 17+)
- Long-term strategies: Sustainable weight maintenance
- Ongoing monitoring: Regular health and sleep assessments
- Lifestyle integration: Healthy habits become automatic
- Prevention focus: Maintain improvements and prevent relapse
Overcoming Common Challenges
Plateaus:
- Reassess calorie needs: Adjust for new weight and activity level
- Change exercise routine: Increase intensity or try new activities
- Review food choices: Ensure accurate calorie counting
- Patience: Plateaus are normal, focus on long-term progress
Sleep Apnea Persistence:
- CPAP compliance: Ensure proper use and maintenance
- Positional therapy: Sleep on side to reduce symptoms
- Nasal treatments: Address nasal congestion issues
- Professional consultation: Regular follow-up with sleep specialist
Motivation Issues:
- Small wins: Celebrate every pound lost and improvement
- Progress photos: Visual reminders of changes
- Support system: Engage family, friends, or support groups
- Professional help: Consider working with a health coach or therapist
Medical Interventions
Weight Loss Medications
Prescription Options:
- Orlistat: Reduces fat absorption from food
- Phentermine: Appetite suppressant (short-term use)
- Liraglutide: GLP-1 agonist, reduces appetite
- Naltrexone-bupropion: Combination medication for weight loss
Considerations:
- Medical supervision: Requires prescription and monitoring
- Side effects: Potential adverse effects and interactions
- Cost: May be expensive and not covered by insurance
- Long-term use: Most medications for short-term use only
Bariatric Surgery
Surgical Options:
- Gastric bypass: Reroutes digestive system, reduces absorption
- Sleeve gastrectomy: Removes portion of stomach
- Gastric banding: Adjustable band around stomach
- Biliopancreatic diversion: More complex procedure
Benefits for Sleep Apnea:
- Significant weight loss: 60-80% excess weight loss
- Sleep apnea improvement: 80-90% show significant improvement
- Metabolic benefits: Improved insulin sensitivity and glucose control
- Quality of life: Major improvements in daily functioning
Considerations:
- Surgical risks: Potential complications and side effects
- Lifestyle changes: Permanent dietary and exercise modifications
- Long-term follow-up: Requires ongoing medical monitoring
- Cost: Expensive procedure, insurance coverage varies
Monitoring Progress
Key Metrics to Track
Weight and Body Composition:
- Body weight: Weekly measurements, same time and conditions
- Body mass index: Calculate BMI regularly
- Neck circumference: Important for sleep apnea risk
- Body fat percentage: More accurate than weight alone
Sleep Quality:
- Apnea-Hypopnea Index (AHI): Measure of sleep apnea severity
- Oxygen saturation: Blood oxygen levels during sleep
- Sleep efficiency: Percentage of time actually sleeping
- Daytime sleepiness: Epworth Sleepiness Scale scores
Health Markers:
- Blood pressure: Regular monitoring, especially morning readings
- Blood glucose: Fasting and post-meal levels
- Cholesterol: Lipid panel including HDL, LDL, triglycerides
- Inflammatory markers: C-reactive protein, other inflammation indicators
Technology Tools
Wearable Devices:
- Fitness trackers: Monitor activity, sleep, and heart rate
- Smart scales: Track weight, body composition, and trends
- Sleep monitors: Track sleep quality and breathing patterns
- Mobile apps: Food tracking, exercise logging, progress monitoring
Professional Monitoring:
- Sleep studies: Periodic assessment of sleep apnea severity
- Medical check-ups: Regular health assessments
- Nutrition counseling: Professional dietary guidance
- Exercise physiology: Fitness assessment and program design
Long-term Success Strategies
Maintaining Weight Loss
Lifestyle Integration:
- Habit formation: Healthy behaviors become automatic
- Regular monitoring: Ongoing assessment of weight and health
- Social support: Maintain connections with supportive people
- Professional relationships: Regular follow-up with healthcare providers
Preventing Relapse:
- Early warning signs: Recognize triggers for weight gain
- Crisis management: Plan for challenging situations
- Flexibility: Allow occasional indulgences without guilt
- Self-compassion: Be kind to yourself during setbacks
Ongoing Health Management
Sleep Apnea Monitoring:
- Regular assessments: Annual sleep studies if symptoms persist
- CPAP maintenance: Regular cleaning and replacement of equipment
- Symptom awareness: Monitor for return of sleep apnea signs
- Professional consultation: Regular follow-up with sleep specialist
Preventive Healthcare:
- Annual physical: Comprehensive health assessment
- Screening tests: Regular cancer and disease screening
- Vaccinations: Stay current with recommended vaccines
- Dental care: Regular dental check-ups and cleaning
Conclusion
The relationship between sleep apnea and weight management is complex but manageable. By understanding the bidirectional nature of this relationship and implementing comprehensive treatment strategies, most people can break the vicious cycle and achieve significant improvements in both sleep quality and overall health.
The key to success is a multifaceted approach that addresses both sleep apnea and weight management simultaneously. This includes medical treatment for sleep apnea, lifestyle modifications for weight loss, and ongoing monitoring to ensure long-term success.
Remember that change takes time and persistence. Start with small, manageable changes and gradually build a comprehensive program that works for your individual needs. With the right approach and support, you can achieve better sleep, improved health, and a higher quality of life.
Key Takeaways
- Sleep apnea and weight have a bidirectional relationship that creates a vicious cycle
- Weight loss of 10-20% can significantly improve sleep apnea symptoms
- Sleep apnea affects hormones that control appetite and metabolism
- Comprehensive treatment should address both sleep apnea and weight management
- Lifestyle changes including diet and exercise are essential for long-term success
- Medical interventions may be needed for severe cases
- Regular monitoring and follow-up are crucial for maintaining improvements
- Breaking the cycle requires patience, persistence, and professional support
References
- American Academy of Sleep Medicine. (2014). International Classification of Sleep Disorders, 3rd Edition.
- National Sleep Foundation. (2020). Sleep in America Poll: Sleep Apnea and Weight.
- Sleep Foundation. (2021). Sleep Apnea and Weight: The Connection.
- Mayo Clinic. (2021). Sleep Apnea and Weight Management.
- Harvard Health Publishing. (2020). Sleep Apnea and Obesity: Breaking the Cycle.
Related Articles
- The Role of Weight and Obesity in Snoring and Sleep Apnea
- Sleep Apnea Solutions: Natural Treatment & Lifestyle Changes
- Sleep Apnea Treatment Options: From CPAP to Lifestyle Changes
