Oral Appliances for Sleep Apnea Treatment: A Non-CPAP Solution
Published by Dr. Emily Thompson | Sleep Medicine and Dental Sleep Medicine Specialist
 Oral appliance therapy for OSA
Oral appliance therapy for OSA
Continuous Positive Airway Pressure (CPAP) therapy has long been the gold standard treatment for sleep apnea, but it's not the right solution for everyone. Many people find CPAP uncomfortable, inconvenient, or simply prefer alternative treatments. Oral appliances offer an effective, comfortable, and portable solution for many sleep apnea patients. This comprehensive guide explores how oral appliances work, who they're suitable for, and how they compare to other treatment options.
Understanding Oral Appliances for Sleep Apnea
What Are Oral Appliances?
Definition:
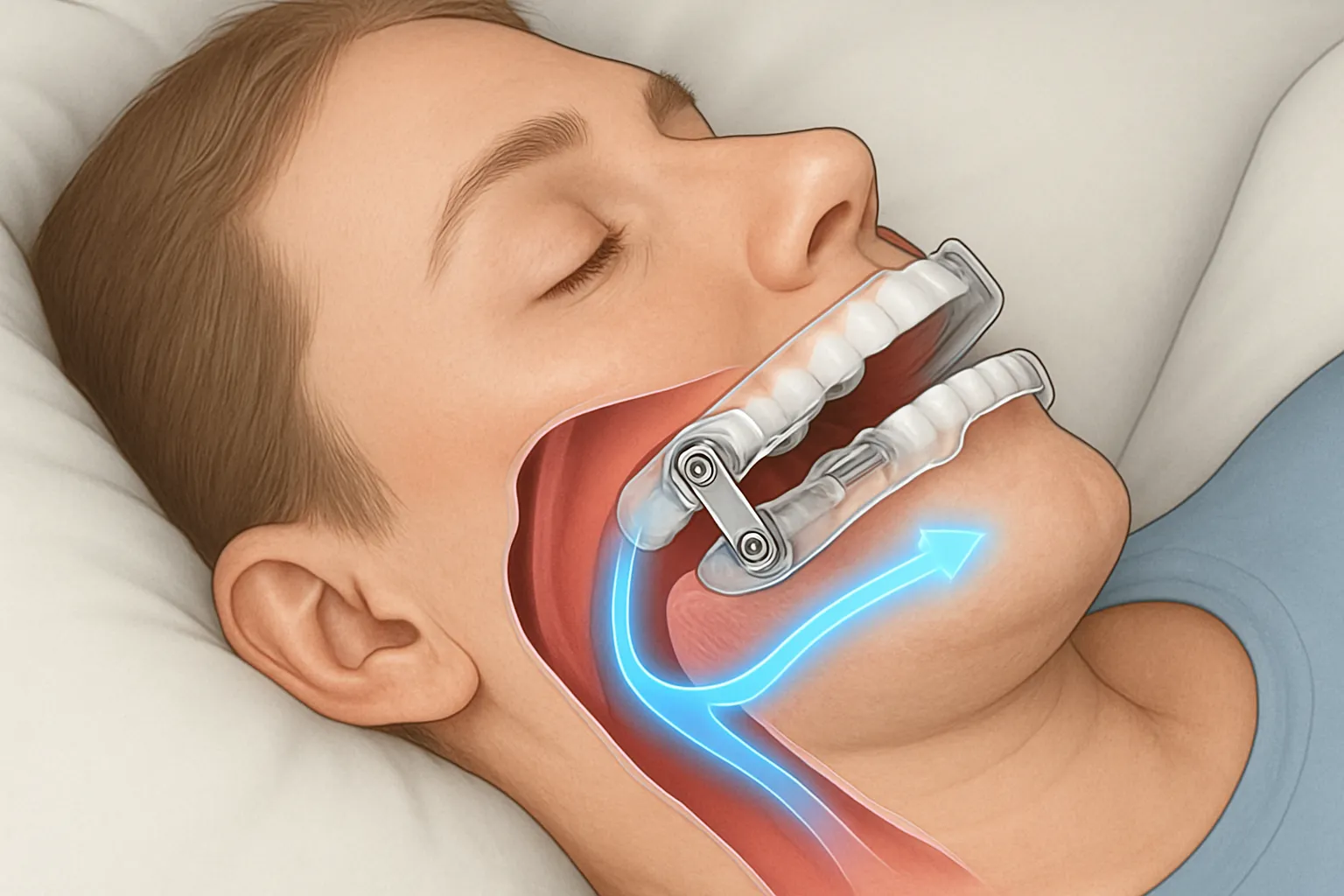
- Oral appliances: Custom-fitted devices worn in the mouth during sleep
- Mechanism: Reposition jaw and tongue to keep airway open
- Types: Mandibular advancement devices, tongue retaining devices
- Customization: Individually fitted by dental sleep medicine specialists
How They Work:
- Jaw repositioning: Move lower jaw forward to open airway
- Tongue control: Prevent tongue from blocking throat
- Muscle tone: Maintain airway muscle tone during sleep
- Airflow improvement: Increase space for air to pass through
Key Components:
- Upper and lower trays: Fit over teeth like mouthguards
- Adjustment mechanism: Allow fine-tuning of jaw position
- Material: Medical-grade acrylic or thermoplastic
- Retention: Secure fit that stays in place during sleep
 Oral appliance in use for sleep apnea
Oral appliance in use for sleep apnea
Types of Oral Appliances
Mandibular Advancement Devices (MADs):
- Most common type: Reposition lower jaw forward
- Adjustable design: Allow gradual advancement over time
- Bilateral design: Connect upper and lower jaws
- Custom fitting: Made from dental impressions
Tongue Retaining Devices (TRDs):
- Tongue control: Hold tongue in forward position
- Suction mechanism: Create vacuum to hold tongue
- Less common: Used when MADs aren't suitable
- Specialized fitting: Require specific tongue measurements
Hybrid Devices:
- Combination approach: Combine multiple mechanisms
- Customizable: Adjustable for individual needs
- Advanced features: May include sensors or monitoring
- Higher cost: More expensive than standard devices
Who Can Benefit from Oral Appliances?
Ideal Candidates
Mild to Moderate Sleep Apnea:
- Apnea-Hypopnea Index (AHI): 5-30 events per hour
- Symptom severity: Mild to moderate daytime sleepiness
- Treatment response: Good response to jaw repositioning
- Compliance: Willing to wear device consistently
Positional Sleep Apnea:
- Position-dependent: Apnea mainly when sleeping on back
- Combination therapy: Oral appliance with positional therapy
- Enhanced effectiveness: Better results than either treatment alone
- Lifestyle compatibility: Fits well with active lifestyle
CPAP Intolerance:
- CPAP discomfort: Unable to tolerate CPAP mask or pressure
- Claustrophobia: Fear of confined spaces or masks
- Travel needs: Difficulty using CPAP while traveling
- Lifestyle factors: Active lifestyle incompatible with CPAP
Contraindications and Limitations
Dental Health Requirements:
- Adequate teeth: Need sufficient teeth for device retention
- Good oral health: No active gum disease or tooth decay
- Stable bite: No major bite problems or jaw issues
- Dental work: May need completion before fitting
Severity Limitations:
- Severe sleep apnea: AHI >30 may not respond adequately
- Complex cases: Multiple anatomical issues may limit effectiveness
- Comorbid conditions: Other sleep disorders may require different treatment
- Individual response: Some people don't respond to oral appliances
Medical Considerations:
- Jaw problems: Temporomandibular joint (TMJ) disorders
- Bruxism: Teeth grinding may damage appliance
- Dental work: Ongoing dental treatment may affect fit
- Medical conditions: Some conditions may contraindicate use
How Oral Appliances Work
Mechanism of Action
Jaw Repositioning:
- Forward movement: Lower jaw moves forward and down
- Airway opening: Creates more space behind tongue
- Muscle tension: Increases muscle tone in airway
- Collapse prevention: Prevents airway from collapsing during sleep
Tongue Control:
- Forward positioning: Holds tongue away from throat
- Space creation: Maintains open passage for air
- Muscle activation: Stimulates airway muscles
- Collapse resistance: Reduces likelihood of airway obstruction
Airway Stabilization:
- Structural support: Provides mechanical support to airway
- Muscle coordination: Improves coordination of breathing muscles
- Pressure distribution: Distributes forces that could collapse airway
- Dynamic adjustment: Adapts to changes in sleep position
Physiological Effects
Airway Dimensions:
- Increased space: More room for air to flow
- Reduced resistance: Less obstruction to breathing
- Improved airflow: Better oxygen delivery to lungs
- Stable breathing: More consistent breathing patterns
Muscle Function:
- Enhanced tone: Better muscle activation during sleep
- Coordination: Improved coordination between breathing muscles
- Strength: Gradual strengthening of airway muscles
- Endurance: Better muscle performance throughout night
Sleep Quality:
- Reduced awakenings: Fewer breathing-related awakenings
- Better sleep stages: More time in restorative sleep
- Oxygen levels: Improved blood oxygen saturation
- Sleep continuity: Less fragmented sleep
Getting Fitted for an Oral Appliance
Initial Consultation
Sleep Medicine Evaluation:
- Sleep study review: Analyze results from sleep study
- Severity assessment: Determine if oral appliance is appropriate
- Treatment planning: Develop comprehensive treatment plan
- Referral coordination: Connect with dental sleep medicine specialist
Dental Assessment:
- Oral health evaluation: Check teeth, gums, and jaw health
- Bite analysis: Assess current bite and jaw position
- Imaging studies: X-rays or scans if needed
- Treatment planning: Plan appliance design and fitting
Patient Education:
- Treatment options: Explain all available treatments
- Expectations: Set realistic expectations for results
- Commitment required: Explain need for consistent use
- Follow-up plan: Outline monitoring and adjustment schedule
Fitting Process
Dental Impressions:
- Mold creation: Make detailed impressions of teeth
- Bite registration: Record current jaw position
- Photographs: Document current appearance
- Measurements: Take precise measurements of mouth
Appliance Fabrication:
- Custom design: Design appliance based on individual needs
- Material selection: Choose appropriate materials
- Adjustment mechanism: Include adjustment capabilities
- Quality control: Ensure proper fit and function
Initial Fitting:
- Trial fitting: Test appliance for comfort and fit
- Adjustment: Make initial adjustments for optimal fit
- Instructions: Provide detailed care and use instructions
- Follow-up scheduling: Plan for adjustments and monitoring
Using Your Oral Appliance
Daily Care and Maintenance
Cleaning Routine:
- Daily cleaning: Clean appliance every morning
- Toothbrush use: Use soft toothbrush and mild soap
- Rinsing: Rinse thoroughly with water
- Drying: Allow to air dry before storage
Storage:
- Protective case: Store in provided case when not in use
- Ventilation: Ensure case has ventilation holes
- Temperature: Keep in cool, dry place
- Protection: Avoid damage from pets or children
Regular Maintenance:
- Inspection: Check for wear or damage regularly
- Professional cleaning: Professional cleaning every 6 months
- Adjustment: Schedule adjustments as needed
- Replacement: Replace when worn or damaged
Wearing Schedule
Initial Adaptation:
- Gradual introduction: Start with short periods during day
- Nighttime use: Begin using during sleep when comfortable
- Adjustment period: Allow 1-2 weeks for adaptation
- Comfort monitoring: Note any discomfort or issues
Regular Use:
- Consistent wear: Use every night for best results
- Travel use: Take appliance when traveling
- Backup plan: Have backup appliance if possible
- Compliance tracking: Monitor usage and effectiveness
Troubleshooting:
- Discomfort: Contact provider for adjustments
- Fit issues: Schedule appointment for refitting
- Damage: Seek professional repair or replacement
- Effectiveness: Monitor sleep quality and symptoms
Effectiveness and Monitoring
Measuring Success
Sleep Study Follow-up:
- Repeat testing: Sleep study after 3-6 months of use
- AHI comparison: Compare before and after AHI values
- Oxygen levels: Assess improvement in oxygen saturation
- Sleep quality: Evaluate improvement in sleep architecture
Symptom Improvement:
- Daytime sleepiness: Reduced sleepiness and fatigue
- Snoring reduction: Decreased or eliminated snoring
- Sleep quality: Better sleep and more restful nights
- Quality of life: Improved daily functioning and mood
Objective Measures:
- Compliance tracking: Monitor actual usage time
- Wear patterns: Track when and how long appliance is worn
- Adjustment needs: Record frequency of adjustments
- Side effects: Monitor for any adverse effects
Long-term Monitoring
Regular Follow-up:
- Dental check-ups: Every 6 months for oral health
- Sleep medicine: Annual review of sleep apnea status
- Appliance assessment: Regular evaluation of appliance condition
- Treatment effectiveness: Ongoing assessment of results
Adjustment Needs:
- Fit changes: Adjustments as teeth or jaw change
- Effectiveness changes: Modifications if effectiveness decreases
- Comfort issues: Adjustments for comfort or fit problems
- Wear patterns: Changes based on usage patterns
Treatment Evolution:
- Severity changes: May need different treatment if apnea worsens
- Lifestyle changes: Adjustments for new circumstances
- Health changes: Modifications for new medical conditions
- Alternative treatments: Consider other options if needed
Comparing Oral Appliances to Other Treatments
vs. CPAP Therapy
Effectiveness:
- Mild to moderate apnea: Similar effectiveness to CPAP
- Severe apnea: CPAP generally more effective
- Individual response: Some people respond better to one or the other
- Compliance: Often better compliance with oral appliances
Comfort and Convenience:
- Portability: Oral appliances much more portable
- Noise: Silent compared to CPAP machines
- Comfort: Often more comfortable than CPAP masks
- Travel: Much easier to use while traveling
Cost Considerations:
- Initial cost: Oral appliances may cost more initially
- Ongoing costs: CPAP has ongoing costs for supplies
- Insurance coverage: Both may be covered by insurance
- Long-term value: Consider total cost over time
vs. Surgery
Effectiveness:
- Reversible: Oral appliances are completely reversible
- Adjustable: Can be modified as needs change
- Surgical risks: No surgical risks or complications
- Recovery time: No recovery period needed
Permanence:
- Temporary solution: Appliance must be worn each night
- Surgical results: Surgery provides permanent structural changes
- Maintenance: Appliance requires ongoing care and maintenance
- Long-term commitment: Surgery is one-time procedure
Risk Profile:
- Low risk: Oral appliances have minimal risks
- Surgical risks: Surgery carries inherent risks
- Complications: Few complications with oral appliances
- Reversibility: Can stop using appliance at any time
Potential Side Effects and Complications
Common Side Effects
Dental Changes:
- Bite changes: Slight changes in how teeth fit together
- Tooth movement: Minor shifting of teeth over time
- Jaw position: Changes in jaw position or alignment
- Temporary effects: Most changes are temporary and reversible
Discomfort:
- Initial soreness: Common during first few weeks
- Jaw stiffness: Morning stiffness that usually resolves
- Tooth sensitivity: Temporary sensitivity to temperature
- Saliva changes: May affect saliva production initially
Sleep-related Issues:
- Drooling: May cause increased drooling initially
- Dry mouth: Can cause dry mouth during sleep
- Gag reflex: May trigger gag reflex in some people
- Sleep disruption: Temporary disruption while adapting
Serious Complications
Jaw Problems:
- TMJ disorders: May worsen existing TMJ problems
- Jaw pain: Persistent pain that doesn't resolve
- Jaw clicking: Clicking or popping sounds
- Limited movement: Reduced jaw opening or movement
Dental Damage:
- Tooth damage: Damage to teeth or dental work
- Gum problems: Irritation or damage to gums
- Bite problems: Significant changes in bite alignment
- Tooth loss: Rare but possible in severe cases
Sleep Apnea Worsening:
- Effectiveness decrease: Appliance may become less effective
- Symptom return: Sleep apnea symptoms may return
- Severity increase: Apnea may become more severe
- Treatment failure: May need to switch to other treatments
When to Seek Professional Help
Adjustment Needs
Fit Problems:
- Loose fit: Appliance feels loose or falls out
- Tight fit: Appliance feels too tight or uncomfortable
- Pain or discomfort: Persistent pain that doesn't improve
- Damage: Visible damage or wear to appliance
Effectiveness Issues:
- Snoring return: Snoring returns or worsens
- Sleepiness return: Daytime sleepiness increases
- Sleep quality: Sleep quality decreases
- Breathing problems: Breathing difficulties return
Side Effects:
- Persistent pain: Pain that continues beyond adaptation period
- Jaw problems: New or worsening jaw problems
- Dental changes: Significant changes in teeth or bite
- Sleep disruption: Ongoing sleep problems
Emergency Situations
Severe Pain:
- Unbearable pain: Pain that prevents sleep or daily activities
- Jaw locking: Jaw becomes stuck or locked
- Severe swelling: Significant swelling in mouth or jaw
- Bleeding: Persistent bleeding from gums or mouth
Breathing Problems:
- Difficulty breathing: New or worsening breathing problems
- Chest pain: Chest pain or pressure
- Dizziness: Lightheadedness or fainting
- Emergency symptoms: Any life-threatening symptoms
Dental Emergencies:
- Broken appliance: Appliance breaks or becomes unusable
- Lost appliance: Appliance is lost or damaged beyond repair
- Dental damage: Significant damage to teeth or mouth
- Infection signs: Signs of infection in mouth or jaw
Conclusion
Oral appliances offer an effective, comfortable, and convenient alternative to CPAP therapy for many people with sleep apnea. They work by repositioning the jaw and tongue to keep the airway open during sleep, providing relief from sleep apnea symptoms without the bulk and noise of CPAP machines.
The key to success with oral appliances is proper fitting, regular monitoring, and consistent use. While they may not be suitable for everyone, they provide an excellent treatment option for people with mild to moderate sleep apnea who find CPAP uncomfortable or inconvenient.
If you're considering an oral appliance for sleep apnea, consult with both a sleep medicine specialist and a dental sleep medicine specialist to determine if this treatment is right for you. With proper care and monitoring, oral appliances can provide long-term relief from sleep apnea and significantly improve your sleep quality and overall health.
Key Takeaways
- Oral appliances are effective for mild to moderate sleep apnea
- They work by repositioning the jaw and tongue to open the airway
- Custom fitting by a dental sleep medicine specialist is essential
- Regular monitoring and adjustments are necessary for optimal results
- They offer advantages in comfort and portability compared to CPAP
- Potential side effects include dental changes and jaw discomfort
- Professional help should be sought for any problems or concerns
- Long-term success requires ongoing care and monitoring
References
- American Academy of Sleep Medicine. (2014). International Classification of Sleep Disorders, 3rd Edition.
- American Academy of Dental Sleep Medicine. (2021). Oral Appliance Therapy for Sleep Apnea.
- Sleep Foundation. (2021). Oral Appliances for Sleep Apnea: What You Need to Know.
- Mayo Clinic. (2021). Oral Appliances for Sleep Apnea.
- Harvard Health Publishing. (2020). Sleep Apnea Treatment Options: Beyond CPAP.
Related Articles
- Sleep Apnea Treatment Options: From CPAP to Lifestyle Changes
- Sleep Apnea Treatment Options Beyond CPAP
- Sleep Apnea Machine: Complete CPAP Therapy Guide
